Anat Cell Biol.
2010 Sep;43(3):260-267. 10.5115/acb.2010.43.3.260.
Tibial intramedullary canal axis and its influence on the intramedullary alignment system entry point in Koreans
- Affiliations
-
- 1Catholic Institute for Applied Anatomy ; Department of Anatomy, School of Medicine, The Catholic University of Korea, Seoul, Korea. hsh@catholic.ac.kr
- 2Somang Orthopedic Clinic, Seoul, Korea.
- KMID: 2168881
- DOI: http://doi.org/10.5115/acb.2010.43.3.260
Abstract
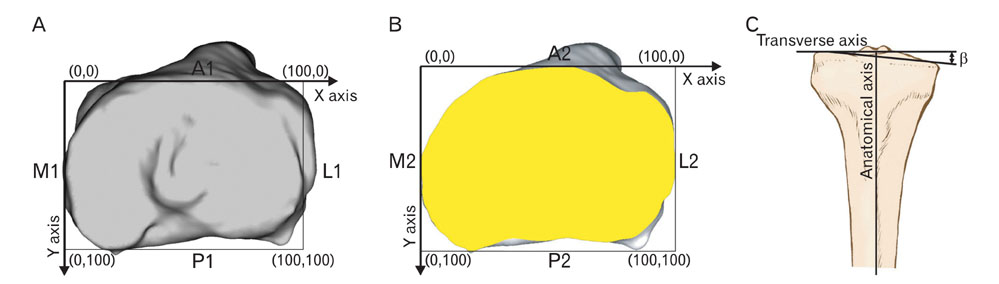
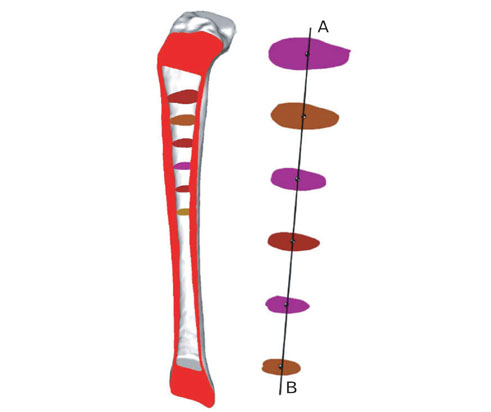
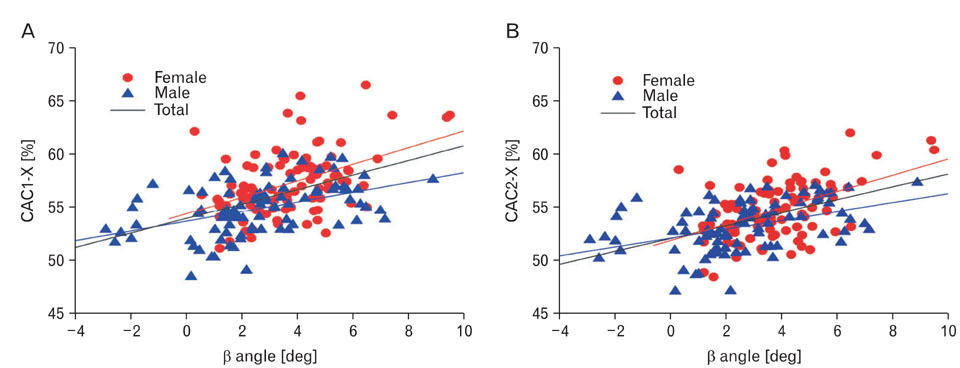
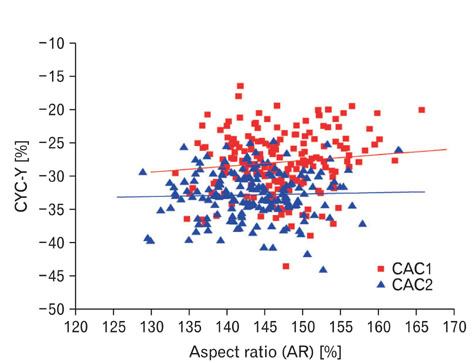
- Using computerized tomographic data and three dimensional model, we studied the influence of tibial intramedullary canal axis and other morphologic factors of the tibia on the entry point for tibial intramedullary alignment guides. Various anatomical parameters including tibial anteroposterior dimensions (AP), mediolateral dimensions (ML), aspect ratio (ML/AP), bowing and the intramedullary canal axis were studied. In addition, the entry point for the intramedullary alignment guide for primary and revision total knee arthroplasty were studied. The averaged entry point at the level of the tibial plateau was 5.7+/-2.2 mm anterior and 4.3+/-2.0 mm lateral to the classical entry point (P<.001). Furthermore, this entry point was more anterolateral in females when compared to males (P<.001). At a depth 10 mm below the tibial plateau, the entry point was on average 8.8+/-1.9 mm anterior and 2.9+/-1.9 mm lateral to the center of the cut surface. With increasing tibial varus the entry point tended to shift laterally at both levels (r=0.49) (P<.001). In Korean, the entry point for tibial intramedullary alignment systems is anterolateral to the classically described entry point. Moreover, the increment of tibial varus necessitates more lateral placement of the entry point. Intraoperatively, the entry point can be localized during primary knee arthroplasty to a point 15.9+/-2.8 mm anterior to and 1.2+/-2.8 mm lateral to the lateral tibial spine. For revision knee arthroplasty the point is on average 8.8+/-1.9 mm anterior and 2.9+/-1.9 mm lateral to the center of the cut surface of the tibia at a depth of 10 mm from the articular surface.
Keyword
Figure
Reference
-
1. Benjamin J. Component alignment in total knee arthroplasty. Instr Course Lect. 2006. 55:405–412.2. Bloebaum RD, Bachus KN, Mitchell W, Hoffman G, Hofmann AA. Analysis of the bone surface area in resected tibia. Implications in tibial component subsidence and fixation. Clin Orthop Relat Res. 1994. 309:2–10.3. Hicks CA, Noble P, Tullos H. The anatomy of the tibial intramedullary canal. Clin Orthop Relat Res. 1995. 321:111–116.4. Ishii Y, Ohmori G, Bechtold JE, Gustilo RB. Extramedullary versus intramedullary alignment guides in total knee arthroplasty. Clin Orthop Relat Res. 1995. 318:167–175.5. Matsui Y, Kadoya Y, Uehara K, Kobayashi A, Takaoka K. Rotational deformity in varus osteoarthritis of the knee: analysis with computed tomography. Clin Orthop Relat Res. 2005. 433:147–151.6. Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988. 226:49–64.7. Scuderi GR, Insall JN. The posterior stabilized knee prosthesis. Orthop Clin North Am. 1989. 20:71–78.8. Westrich GH, Haas SB, Insall JN, Frachie A. Resection specimen analysis of proximal tibial anatomy based on 100 total knee arthroplasty specimens. J Arthroplasty. 1995. 10:47–51.9. Whiteside LA, Summers RG. Anatomic landmarks for an intramedullary alignment system for total knee replacement. Orthop Trans. 1983. 7:546–547.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three Dimensional Analysis for the Intramedullary Canal Axis of the Proximal Tibia: Clinical Relevance to Total Knee Arthroplasty
- Total Knee Arthroplasty using Intramedullary Tibial Cutting Guide
- Extramedullary Versus Intramedullary Alignment Guide Systems in Total Knee Arthroplasty
- A Bent Intramedullary Interlocking Tibial Nail: A Case Report
- Posterior Cortical Fracture of Tibia during Tibial Interlocking Intramedurally Nail Extraction : A report of 3 cases