Electrolyte Blood Press.
2012 Dec;10(1):12-17. 10.5049/EBP.2012.10.1.12.
Novel Biomarkers for Cardio-renal Syndrome
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Kyung Hee University, Seoul, Korea. khjeong@khu.ac.kr
- KMID: 2168389
- DOI: http://doi.org/10.5049/EBP.2012.10.1.12
Abstract
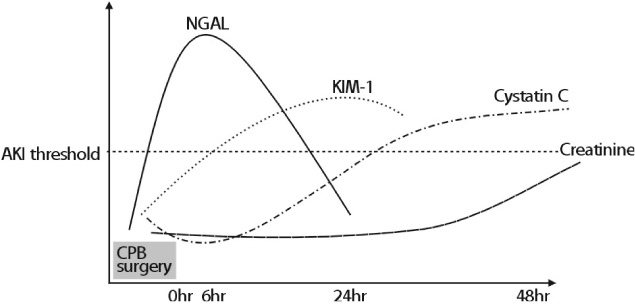
- Cardio-renal syndrome (CRS) is a frequent and life-threatening syndrome. It is a disorder of the heart and kidneys in which acute or chronic dysfunction in one organ may induce acute or chronic dysfunction in the other organ. Acute kidney injury (AKI) is strongly associated with increased morbidity and mortality in patients with CRS. Early detection of renal dysfunction is not possible using the traditional marker, serum creatinine, and therefore efforts to explore possible biomarkers for early detection of AKI are being made. Apart from predicting AKI, several biomarker studies also identified predictors for poor prognosis such as the need for renal replacement therapy (RRT) or death. It is possible that biomarkers can become risk factors in an improvement of clinical outcomes of CRS. Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in patients with renal dysfunction and the treatment for this disease can be modified based on cardiac biomarkers. In addition to natriuretic peptides, which are established cardiac markers, several new biomarkers have been identified and may play important roles in CRS. In this review, we will briefly summarize the literature on novel renal and cardiac biomarkers and discuss their potential roles in the clinical outcome of CRS.
MeSH Terms
Figure
Reference
-
1. Flower DR, North AC, Attwood TK. Structure and sequence relationships in the lipocalins and related proteins. Protein Sci. 1993. 2:753–761.
Article2. Mishra J, Dent C, Tarabishi R, et al. Neutrophil gelatinaseassociated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005. 365:1231–1238.
Article3. Mishra J, Ma Q, Prada A, et al. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003. 14:2534–2543.
Article4. Mishra J, Mori K, Ma Q, Kelly C, Barasch J, Devarajan P. Neutrophil gelatinase-associated lipocalin: a novel early urinary biomarker for cisplatin nephrotoxicity. Am J Nephrol. 2004. 24:307–315.
Article5. Cruz DN, Fard A, Clementi A, Ronco C, Maisel A. Role of biomarkers in the diagnosis and management of cardio-renal syndromes. Semin Nephrol. 2012. 32:79–92.
Article6. Alvelos M, Pimentel R, Pinho E, et al. Neutrophil gelatinase-associated lipocalin in the diagnosis of type 1 cardiorenal syndrome in the general ward. Clin J Am Soc Nephrol. 2011. 6:476–481.
Article7. Shaker OG, El-Shehaby A, El-Khatib M. Early diagnostic markers for contrast nephropathy in patients undergoing coronary angiography. Angiology. 2010. 61:731–736.
Article8. Han WK, Wagener G, Zhu Y, Wang S, Lee HT. Urinary biomarkers in the early detection of acute kidney injury after cardiac surgery. Clin J Am Soc Nephrol. 2009. 4:873–882.
Article9. Damman K, van Veldhuisen DJ, Navis G, Voors AA, Hillege HL. Urinary neutrophil gelatinase associated lipocalin (NGAL), a marker of tubular damage, is increased in patients with chronic heart failure. Eur J Heart Fail. 2008. 10:997–1000.
Article10. Yndestad A, Landro L, Ueland T, et al. Increased systemic and myocardial expression of neutrophil gelatinase-associated lipocalin in clinical and experimental heart failure. Eur Heart J. 2009. 30:1229–1236.
Article11. Liangos O, Tighiouart H, Perianayagam MC, et al. Comparative analysis of urinary biomarkers for early detection of acute kidney injury following cardiopulmonary bypass. Biomarkers. 2009. 14:423–431.
Article12. Malyszko J, Bachorzewska-Gajewska H, Poniatowski B, Malyszko JS, Dobrzycki S. Urinary and serum biomarkers after cardiac catheterization in diabetic patients with stable angina and without severe chronic kidney disease. Ren Fail. 2009. 31:910–919.
Article13. Damman K, Van Veldhuisen DJ, Navis G, et al. Tubular damage in chronic systolic heart failure is associated with reduced survival independent of glomerular filtration rate. Heart. 2010. 96:1297–1302.
Article14. Koyner JL, Vaidya VS, Bennett MR, et al. Urinary biomarkers in the clinical prognosis and early detection of acute kidney injury. Clin J Am Soc Nephrol. 2010. 5:2154–2165.
Article15. Wang QP, Gu JW, Zhan XH, Li H, Luo XH. Assessment of glomerular filtration rate by serum cystatin C in patients undergoing coronary artery bypass grafting. Ann Clin Biochem. 2009. 46:495–500.
Article16. Lassus JP, Nieminen MS, Peuhkurinen K, et al. Markers of renal function and acute kidney injury in acute heart failure: definitions and impact on outcomes of the cardiorenal syndrome. Eur Heart J. 2010. 31:2791–2798.
Article17. Tang WH, Van Lente F, Shrestha K, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail. 2008. 14:394–399.
Article18. Gibey R, Dupond JL, Alber D, Leconte des Floris R, Henry JC. Predictive value of urinary N-acetyl-beta-D-glucosaminidase (NAG), alanine-aminopeptidase (AAP) and beta-2-microglobulin (beta 2M) in evaluating nephrotoxicity of gentamicin. Clin Chim Acta. 1981. 116:25–34.
Article19. Westhuyzen J, Endre ZH, Reece G, Reith DM, Saltissi D, Morgan TJ. Measurement of tubular enzymuria facilitates early detection of acute renal impairment in the intensive care unit. Nephrol Dial Transplant. 2003. 18:543–551.
Article20. Parikh CR, Jani A, Mishra J, et al. Urine NGAL and IL-18 are predictive biomarkers for delayed graft function following kidney transplantation. Am J Transplant. 2006. 6:1639–1645.
Article21. Liang XL, Liu SX, Chen YH, et al. Combination of urinary kidney injury molecule-1 and interleukin-18 as early biomarker for the diagnosis and progressive assessment of acute kidney injury following cardiopulmonary bypass surgery: a prospective nested case-control study. Biomarkers. 2010. 15:332–339.
Article22. McIlroy DR, Wagener G, Lee HT. Biomarkers of acute kidney injury: an evolving domain. Anesthesiology. 2010. 112:998–1004.23. DeFilippi CR, Fink JC, Nass CM, Chen H, Christenson R. N-terminal pro-B-type natriuretic peptide for predicting coronary disease and left ventricular hypertrophy in asymptomatic CKD not requiring dialysis. Am J Kidney Dis. 2005. 46:35–44.
Article24. Goto T, Takase H, Toriyama T, et al. Increased circulating levels of natriuretic peptides predict future cardiac event in patients with chronic hemodialysis. Nephron. 2002. 92:610–615.
Article25. Sommerer C, Beimler J, Schwenger V, et al. Cardiac biomarkers and survival in haemodialysis patients. Eur J Clin Invest. 2007. 37:350–356.
Article26. Luchner A, Hengstenberg C, Lowel H, Riegger GA, Schunkert H, Holmer S. Effect of compensated renal dysfunction on approved heart failure markers: direct comparison of brain natriuretic peptide (BNP) and N-terminal pro-BNP. Hypertension. 2005. 46:118–123.
Article27. Apple FS, Murakami MM, Pearce LA, Herzog CA. Multi-biomarker risk stratification of N-terminal pro-B-type natriuretic peptide, high-sensitivity C-reactive protein, and cardiac troponin T and I in end-stage renal disease for all-cause death. Clin Chem. 2004. 50:2279–2285.
Article28. Carr SJ, Bavanandan S, Fentum B, Ng L. Prognostic potential of brain natriuretic peptide (BNP) in predialysis chronic kidney disease patients. Clin Sci (Lond). 2005. 109:75–82.
Article29. Satyan S, Light RP, Agarwal R. Relationships of N-terminal pro-B-natriuretic peptide and cardiac troponin T to left ventricular mass and function and mortality in asymptomatic hemodialysis patients. Am J Kidney Dis. 2007. 50:1009–1019.
Article30. Troughton RW, Frampton CM, Yandle TG, Espiner EA, Nicholls MG, Richards AM. Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N-BNP) concentrations. Lancet. 2000. 355:1126–1130.
Article31. Jourdain P, Jondeau G, Funck F, et al. Plasma brain natriuretic peptide-guided therapy to improve outcome in heart failure: the STARS-BNP Multicenter Study. J Am Coll Cardiol. 2007. 49:1733–1739.
Article32. Apple FS, Murakami MM, Pearce LA, Herzog CA. Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease. Circulation. 2002. 106:2941–2945.
Article33. Aviles RJ, Askari AT, Lindahl B, et al. Troponin T levels in patients with acute coronary syndromes, with or without renal dysfunction. N Engl J Med. 2002. 346:2047–2052.
Article34. Mallamaci F, Zoccali C, Parlongo S, et al. Troponin is related to left ventricular mass and predicts all-cause and cardiovascular mortality in hemodialysis patients. Am J Kidney Dis. 2002. 40:68–75.
Article35. K/DOQI Workgroup. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis. 2005. 45:S1–S153.