Electrolyte Blood Press.
2011 Dec;9(2):63-66. 10.5049/EBP.2011.9.2.63.
Volume Control by Using the Body Composition Monitor in a Puerperal Patient on Hemodialysis
- Affiliations
-
- 1Department of Internal Medicine, Gachon University of Medicine and Science, Incheon, Korea.
- 2Department of Obstetrics and Gynecology, Gachon University of Medicine and Science, Incheon, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. imsejoong@daum.net
- KMID: 2168386
- DOI: http://doi.org/10.5049/EBP.2011.9.2.63
Abstract
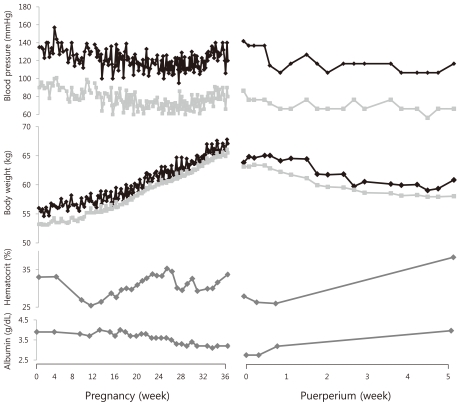
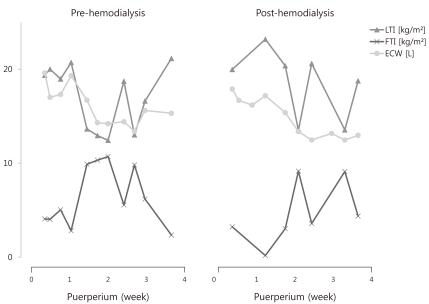
- Accurate measurement of the volume status in hemodialysis patients is important as it can affect mortality. However, no studies have been conducted regarding volume management in cases where a sudden change of body fluid occurs, such as during puerperium in hemodialysis patients. This report presents a case in which the patient was monitored for her body composition and her volume status was controlled using a body composition monitor (BCM) during the puerperal period. This case suggests that using a BCM for volume management may help maintain hemodynamic stability in patients with a rapidly changing volume status for a short term period, such as during puerperium.
MeSH Terms
Figure
Reference
-
1. Kalantar-Zadeh K, Abbott KC, Kronenberg F, Anker SD, Horwich TB, Fonarow GC. Epidemiology of dialysis patients and heart failure patients. Semin Nephrol. 2006; 26:118–133. PMID: 16530605.
Article2. Kalantar-Zadeh K, Regidor DL, Kovesdy CP, et al. Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation. 2009; 119:671–679. PMID: 19171851.
Article3. Zhou YL, Liu J, Sun F, et al. Calf bioimpedance ratio improves dry weight assessment and blood pressure control in hemodialysis patients. Am J Nephrol. 2010; 32:109–116. PMID: 20558982.
Article4. Frank Peacock W, Soto KM. Current technique of fluid status assessment. Congest Heart Fail. 2010; 16(Suppl 1):S45–S51. PMID: 20653711.
Article5. Devolder I, Verleysen A, Vijt D, Vanholder R, Van Biesen W. Body composition, hydration, and related parameters in hemodialysis versus peritoneal dialysis patients. Perit Dial Int. 2010; 30:208–214. PMID: 20081049.
Article6. Machek P, Jirka T, Moissl U, Chamney P, Wabel P. Guided optimization of fluid status in haemodialysis patients. Nephrol Dial Transplant. 2010; 25:538–544. PMID: 19793930.
Article7. Theunissen IM, Parer JT. Fluid and electrolytes in pregnancy. Clin Obstet Gynecol. 1994; 37:3–15. PMID: 8194213.
Article8. Scott DE. Anemia in pregnancy. Obstet Gynecol Annu. 1972; 1:219–244. PMID: 4591070.9. Cho GJ, Yoon HJ, Kim EJ, Oh MJ, Seo HS, Kim HJ. Postpartum changes in body composition. Obesity (Silver Spring). 2011; 19:2425–2428. PMID: 21701569.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical usefulness of bioimpedance analysis for assessing volume status in patients receiving maintenance dialysis
- Hydration Status and Clinical Features in Patients with End-Stage Renal Disease on Regular Hemodialysis
- Overhydration measured by bioimpedance analysis and the survival of patients on maintenance hemodialysis: a single-center study
- Dermographism ( II ) : The Prevalence in Korean Pregnant and Puerperal Women
- Utility of Bioelectrical Impedance Analysis for Body Composition Assessment