Imaging Sci Dent.
2013 Mar;43(1):17-23. 10.5624/isd.2013.43.1.17.
Assessment of the role of cone beam computed sialography in diagnosing salivary gland lesions
- Affiliations
-
- 1Oral and Maxillofacial Radiology, Faculty of Oral and Dental Medicine, Cairo University, Cairo, Egypt.
- 2Oral and Maxillofacial Radiology, Faculty of Dentistry, Minia University, El Menia City, Egypt. mahaeshaq2@yahoo.com
- KMID: 2167442
- DOI: http://doi.org/10.5624/isd.2013.43.1.17
Abstract
- PURPOSE
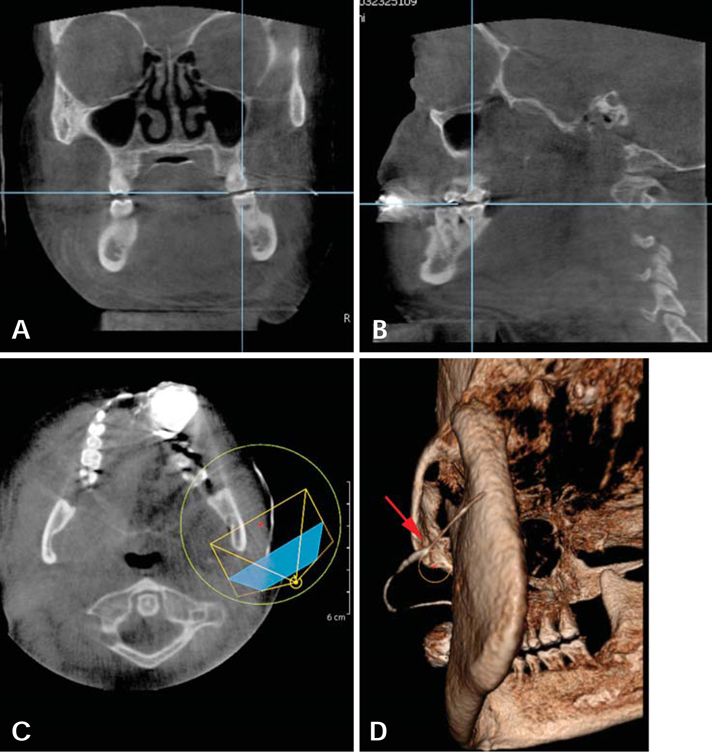
The purpose of this study was to assess cone-beam computed (CBCT) sialography imaging in the detection of different changes associated with lesions of salivary glands.
MATERIALS AND METHODS
This study consisted of 8 cases with signs and symptoms from salivary gland lesions. Conventional sialography using digital panoramic and lateral oblique radiographs and CBCT sialography were performed for each subject. The radiographs were evaluated by 3 radiologists independently of each other. The results were compared between conventional sialography and CBCT sialography in the evaluation of various lesions associated with the salivary glands.
RESULTS
There was an agreement between the radiologists in interpreting the lesions that affected salivary glands with both techniques. The detection of the presence of stones or filling defects, stenosis, ductal evagination, dilatation, and space occupying lesions was 83% for conventional sialography compared with CBCT sialography. CBCT sialography was superior to conventional sialography in revealing stones, stenosis, and strictures, especially in the second and third order branches.
CONCLUSION
It would be advisable to perform CBCT sialography in cases of obstructive salivary gland diseases for better demonstration of the ductal system of the gland.
MeSH Terms
Figure
Cited by 1 articles
-
Therapeutic effect of intraductal irrigation of the salivary gland: A technical report
Chena Lee, Jo-Eun Kim, Kyoung-Hoe Huh, Won-Jin Yi, Min-Suk Heo, Sam-Sun Lee, Soon-Chul Choi
Imaging Sci Dent. 2017;47(2):123-127. doi: 10.5624/isd.2017.47.2.123.
Reference
-
1. Jäger L, Menauer F, Holzknecht N, Scholz V, Grevers G, Reiser M. Sialolithiasis: MR sialography of the submandibular duct - an alternative to conventional sialography and US? Radiology. 2000. 216:665–671.2. Burke CJ, Thomas RH, Howlett D. Imaging the major salivary glands. Br J Oral Maxillofac Surg. 2011. 49:261–269.
Article3. Levy DM, ReMine WH, Devine KD. Salivary gland calculi. Pain, swelling associated with eating. JAMA. 1962. 181:1115–1119.4. Yousem DM, Kraut MA, Chalian AA. Major salivary gland imaging. Radiology. 2000. 216:19–29.
Article5. Rinast E, Gmelin E, Hollands-Thorn B. Digital subtraction sialography, conventional sialography, high-resolution ultrasonography and computed tomography in the diagnosis of salivary gland diseases. Eur J Radiol. 1989. 9:224–230.6. Eracleous E, Kallis S, Tziakouri C, Blease S, Gourtsoyiannis N. Sonography, CT, CT sialography, MRI and MRI sialography in investigation of the facial nerve and the differentiation between deep and superficial parotid lesions. Neuroradiology. 1997. 39:506–511.
Article7. Szolar DH, Groell R, Braun H, Preidler K, Stiskal M, Kern R, et al. Ultrafast computed tomography and three-dimensional image processing of CT sialography in patients with parotid masses poorly defined by magnetic resonance imaging. Acta Otolaryngol. 1996. 116:112–118.
Article8. Szolar DH, Groell R, Preidler K, Braun H, Stiskal MA, Stammberger H, et al. Three-dimensional processing of ultrafast CT sialography for parotid masses. AJNR Am J Neuroradiol. 1995. 16:1889–1893.9. Yajima A, Otonari-Yamamoto M, Sano T, Hayakawa Y, Otonari T, Tanabe K, et al. Cone-beam CT (CB Throne) applied to dentomaxillofacial region. Bull Tokyo Dent Coll. 2006. 47:133–141.
Article10. Drage NA, Brown JE. Cone beam computed sialography of sialoliths. Dentomaxillofac Radiol. 2009. 38:301–305.
Article11. Gritzmann N. Sonography of the salivary glands. AJR Am J Roentgenol. 1989. 153:161–166.
Article12. Avrahami E, Englender M, Chen E, Shabtay D, Katz R, Harell M. CT of submandibular gland sialolithiasis. Neuroradiology. 1996. 38:287–290.
Article13. Ngu RK, Brown JE, Whaites EJ, Drage NA, Ng SY, Makdissi J. Salivary duct strictures: nature and incidence in benign salivary obstruction. Dentomaxillofac Radiol. 2007. 36:63–67.
Article14. Salerno S, Cannizzaro F, Comparetto A, Speciale R, Lo Casto A. Sialographic findings in Wharton duct evagination. Dentomaxillofac Radiol. 2009. 38:550–553.
Article15. Li B, Long X, Cheng Y, Wang S. Cone beam CT sialography of Stafne bone cavity. Dentomaxillofac Radiol. 2011. 40:519–523.
Article16. Licitra L, Grandi C, Prott FJ, Schornagel JH, Bruzzi P, Molinari R. Major and minor salivary glands tumours. Crit Rev Oncol Hematol. 2003. 45:215–225.
Article17. Brown JE. Interventional sialography and minimally invasive techniques in benign salivary gland obstruction. Semin Ultrasound CT MR. 2006. 27:465–475.
Article18. Murray ME, Buckenham TM, Joseph AE. The role of ultrasound in screening patients referred for sialography: a possible protocol. Clin Otolaryngol Allied Sci. 1996. 21:21–23.
Article19. Haring JI. Diagnosing salivary stones. J Am Dent Assoc. 1991. 122:75–76.
Article20. Rzymska-Grala I, Stopa Z, Grala B, Gołębiowski M, Wanyura H, Zuchowska A, et al. Salivary gland calculi - contemporary methods of imaging. Pol J Radiol. 2010. 75:25–37.21. Sumi M, Izumi M, Yonetsu K, Nakamura T. The MR imaging assessment of submandibular gland sialoadenitis secondary to sialolithiasis: correlation with CT and histopathologic findings. AJNR Am J Neuroradiol. 1999. 20:1737–1743.22. Thoeny HC. Imaging of salivary gland tumours. Cancer Imaging. 2007. 7:52–62.
Article23. Lee YY, Wong KT, King AD, Ahuja AT. Imaging of salivary gland tumours. Eur J Radiol. 2008. 66:419–436.
Article24. Jadu F, Yaffe MJ, Lam EW. A comparative study of the effective radiation doses from cone beam computed tomography and plain radiography for sialography. Dentomaxillofac Radiol. 2010. 39:257–263.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multilocular developmental salivary gland defect
- Three-dimensional cone-beam computed tomographic sialography in the diagnosis and management of primary Sjögren syndrome: Report of 3 cases
- Sialography
- Three-dimensional imaging modalities in endodontics
- Developmental salivary gland depression in the ascending mandibular ramus: A cone-beam computed tomography study