Clin Exp Otorhinolaryngol.
2016 Mar;9(1):80-84. 10.21053/ceo.2016.9.1.80.
Metastases of Melanoma to Head and Neck Mucosa: A Report of Short Series
- Affiliations
-
- 1Department of Clinical and Preventive Dentistry, Oral Pathology Section, School of Dentistry, Federal University of Pernambuco, Recife, Brazil. danyel.perez@ufpe.br
- 2Department of Stomatology, A. C. Camargo Cancer Center, São Paulo, Brazil.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, A. C. Camargo Cancer Center, São Paulo, Brazil.
- KMID: 2166294
- DOI: http://doi.org/10.21053/ceo.2016.9.1.80
Abstract
OBJECTIVES
Metastasis of melanoma to the head and neck mucosa is a very unusual condition. The aim of this study was to report four cases of patients with metastatic melanoma in the head and neck mucosa treated at a single institution.
METHODS
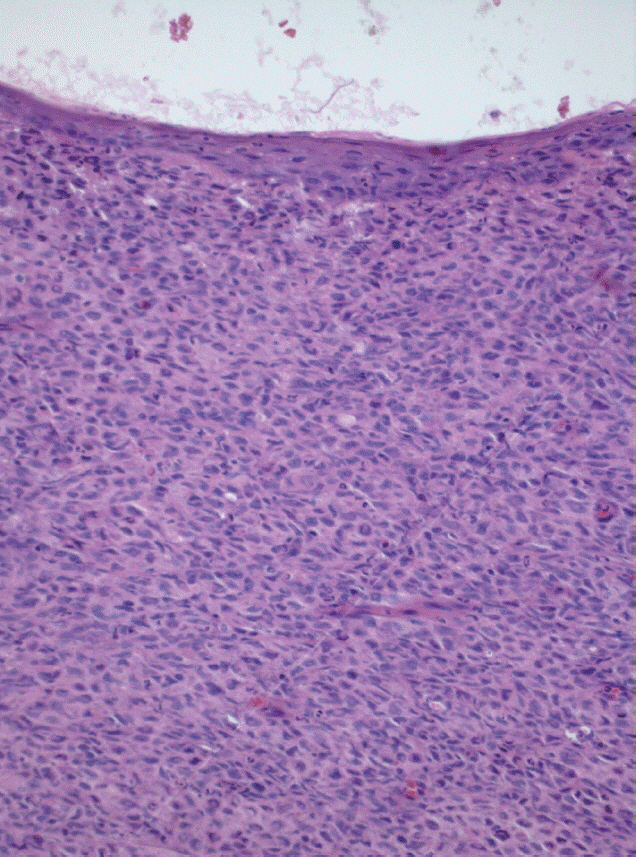
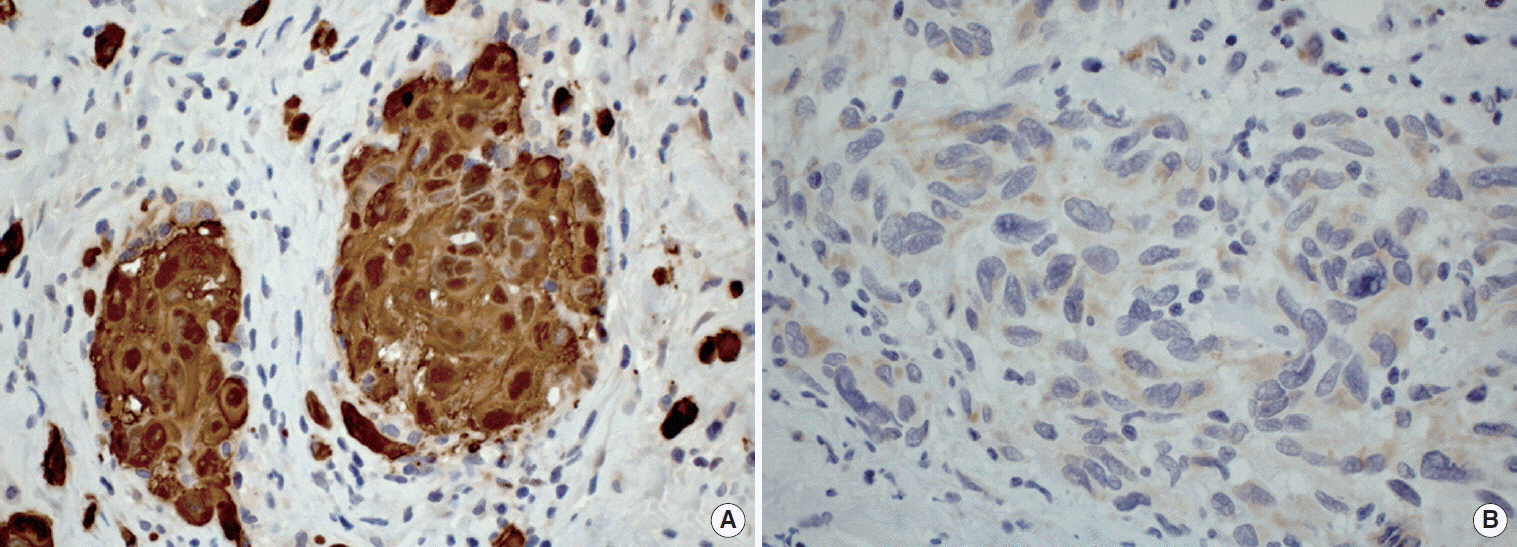
Clinical data were obtained from the medical records. All cases were histologically reviewed to confirm the diagnosis, and immunohistochemical reactions were performed in the cases submitted to biopsy.
RESULTS
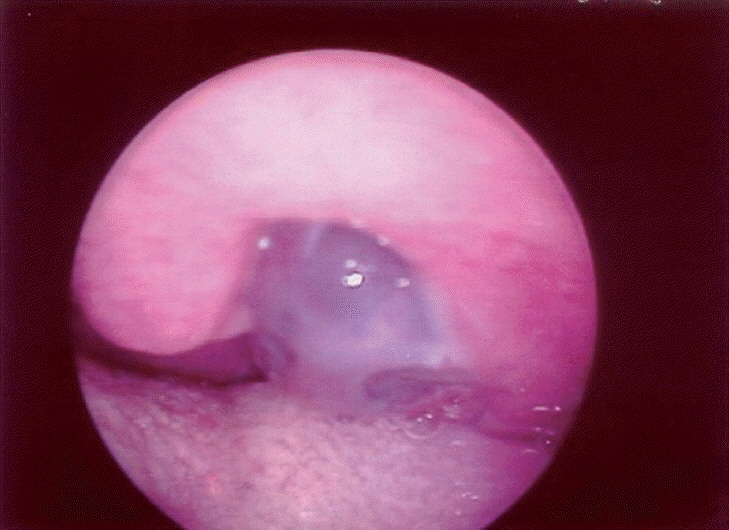
All patients were males and the mean age was 40.5 years old. The sites of the metastatic tumors were gingival mucosa, floor of the mouth, oropharynx, and larynx. Two tumors appeared as submucosal nodules with normal color; one lesion was a blackish nodular lesion, and one was shown to be an ulcerated lesion. The size of tumors ranged from 2.0 to 4.0 cm. All patients had developed systemic disease at time of diagnosis of metastatic tumor in the head and neck mucosa. Survival rates ranged from 2 to 19 months after the diagnosis of the metastatic mucosal melanoma in the head and neck region.
CONCLUSION
Although rare, patients with melanoma must be closely and regularly followed up, with careful routine examination of head and neck, because metastatic tumors in this region seem to be part of a lethal widespread metastatic disease.
MeSH Terms
Figure
Reference
-
1. Lengyel E, Gilde K, Remenar E, Esik O. Malignant mucosal melanoma of the head and neck. Pathol Oncol Res. 2003; 9(1):7–12.2. Patrick RJ, Fenske NA, Messina JL. Primary mucosal melanoma. J Am Acad Dermatol. 2007; May. 56(5):828–34.
Article3. Henderson LT, Robbins KT, Weitzner S. Upper aerodigestive tract metastases in disseminated malignant melanoma. Arch Otolaryngol Head Neck Surg. 1986; Jun. 112(6):659–63.
Article4. Billings KR, Wang MB, Sercarz JA, Fu YS. Clinical and pathologic distinction between primary and metastatic mucosal melanoma of the head and neck. Otolaryngol Head Neck Surg. 1995; Jun. 112(6):700–6.
Article5. Aydogan LB, Myers JN, Myers EN, Kirkwood J. Malignant melanoma metastatic to the tonsil. Laryngoscope. 1996; Mar. 106(3 Pt 1):313–6.
Article6. Coehlo FH, Pellicioli AC, Martins MA, Pavesi VC, Schmerling RA, Martins MD. Multiple metastases of malignant melanoma in the head and neck: a case report and literature review. Gen Dent. 2014; Jan-Feb. 62(1):43–8.7. Mifsud M, Padhya TA. Metastatic melanoma to the upper aerodigestive tract: a systematic review of the literature. Laryngoscope. 2014; May. 124(5):1143–9.8. Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R. Metastatic tumours to the oral cavity: pathogenesis and analysis of 673 cases. Oral Oncol. 2008; Aug. 44(8):743–52.9. Khan KH, Goody RB, Hameed H, Jalil A, Coyle VM, McAleer JJ. Metastatic melanoma: a regional review and future directions. Tumori. 2012; Sep-Oct. 98(5):575–80.
Article10. Larson DL, Larson JD. Head and neck melanoma. Clin Plast Surg. 2010; Jan. 37(1):73–7.
Article11. Bombelli FB, Webster CA, Moncrieff M, Sherwood V. The scope of nanoparticle therapies for future metastatic melanoma treatment. Lancet Oncol. 2014; Jan. 15(1):e22–32.
Article12. Morgan AH, Norris JW, Hicks JN. Palliative laser surgery for melanoma metastatic to the larynx: report of two cases. Laryngoscope. 1985; Jul. 95(7 Pt 1):794–7.13. Mouawad R, Sebert M, Michels J, Bloch J, Spano JP, Khayat D. Treatment for metastatic malignant melanoma: old drugs and new strategies. Crit Rev Oncol Hematol. 2010; Apr. 74(1):27–39.
Article14. Katz KA, Jonasch E, Hodi FS, Soiffer R, Kwitkiwski K, Sober AJ, et al. Melanoma of unknown primary: experience at Massachusetts General Hospital and Dana-Farber Cancer Institute. Melanoma Res. 2005; Feb. 15(1):77–82.
Article15. de Waal AC, Aben KK, van Rossum MM, Kiemeney LA. Melanoma of unknown primary origin: a population-based study in the Netherlands. Eur J Cancer. 2013; Feb. 49(3):676–83.
Article16. Schlagenhauff B, Stroebel W, Ellwanger U, Meier F, Zimmermann C, Breuninger H, et al. Metastatic melanoma of unknown primary origin shows prognostic similarities to regional metastatic melanoma: recommendations for initial staging examinations. Cancer. 1997; Jul. 1. 80(1):60–5.17. Kamposioras K, Pentheroudakis G, Pectasides D, Pavlidis N. Malignant melanoma of unknown primary site. To make the long story short. A systematic review of the literature. Crit Rev Oncol Hematol. 2011; May. 78(2):112–26.
Article18. O’Neill JK, Khundar R, Knowles L, Scott-Young N, Orlando A. Melanoma with an unknown primary: a case series. J Plast Reconstr Aesthet Surg. 2010; Dec. 63(12):2071–80.19. Wang BY, Lawson W, Robinson RA, Perez-Ordonez B, Brandwein M. Malignant melanomas of the parotid: comparison of survival for patients with metastases from known vs unknown primary tumor sites. Arch Otolaryngol Head Neck Surg. 1999; Jun. 125(6):635–9.20. Prens SP, van der Ploeg AP, van Akkooi AC, van Montfort CA, van Geel AN, de Wilt JH, et al. Outcome after therapeutic lymph node dissection in patients with unknown primary melanoma site. Ann Surg Oncol. 2011; Dec. 18(13):3586–92.
Article21. Weide B, Faller C, Elsasser M, Buttner P, Pflugfelder A, Leiter U, et al. Melanoma patients with unknown primary site or nodal recurrence after initial diagnosis have a favourable survival compared to those with synchronous lymph node metastasis and primary tumour. PLoS One. 2013; Jun. 25. 8(6):e66953.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of primary malignant melanoma of hard palate mucosa
- A Case of Desmoplastic Malignant Melanoma
- A Case of Metastatic Malignant Melanoma Presenting as Subcutaneous Posterior Neck Mass
- Comparison Study for Mucosal Malignant Melanoma ofHead and Neck according to Primary Sites
- Two Cases of Malignant Melanoma with Nodal Metastasis from Unknown Primary Site