Clin Endosc.
2013 Sep;46(5):582-585.
Gastric Somatostatinoma: An Extremely Rare Cause of Upper Gastrointestinal Bleeding
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Siriraj Hospital, Mahidol University Faculty of Medicine, Bangkok, Thailand. kaiyjr@gmail.com
- 2Liver and Digestive Institute, Samitivej Sukhumvit Hospital, Bangkok, Thailand.
- 3Department of Pathology, Siriraj Hospital, Mahidol University Faculty of Medicine, Bangkok, Thailand.
Abstract
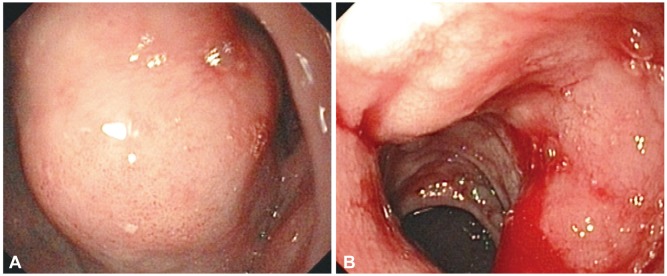
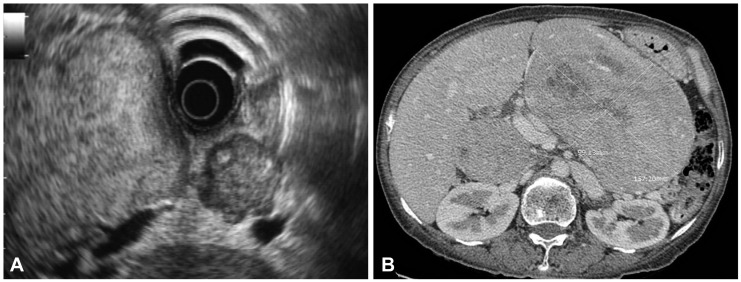
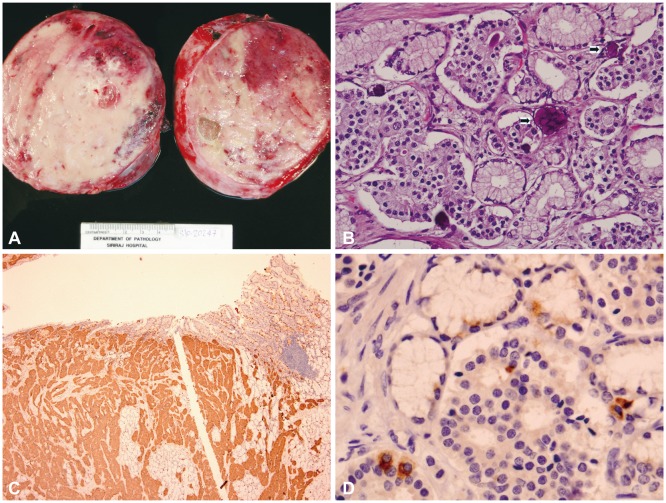
- A 49-year-old woman presented with chronic abdominal discomfort, significant weight loss, and chronic intermittent diarrhea. She suddenly developed massive upper gastrointestinal bleeding and was referred for further treatment. Endoscopy indicated a large mass in the upper gastric body with antral and duodenal bulb involvement. Endosonography showed a large well-defined isoechoic gastric subepithelial mass with multiple intra-abdominal and peripancreatic lymphadenopathy, suspected to be malignant on the basis of fine needle aspiration cytology. The tumor was surgically removed, and histopathology showed typical characteristics of a neuroendocrine tumor. On the basis of immunohistochemical staining, somatostatinoma, a rare neuroendocrine tumor, was diagnosed. Gastrointestinal bleeding is a rare presentation and the stomach is an uncommon tumor location.
MeSH Terms
Figure
Reference
-
1. Larsson LI, Hirsch MA, Holst JJ, et al. Pancreatic somatostatinoma: clinical features and physiological implications. Lancet. 1977; 1:666–668. PMID: 66472.2. Zhang ZY, Zhang R, Wang L, et al. Diagnosis and treatment of pancreatic somatostatinoma: a case report. Chin Med J (Engl). 2008; 121:2363–2365. PMID: 19080351.
Article3. Pernet C, Kluger N, Du-Thanh A, et al. Somatostatin-producing endocrine tumour of the duodenum associated with type 1 neurofibromatosis. Acta Derm Venereol. 2010; 90:320–321. PMID: 20526564.
Article4. Arima H, Natsugoe S, Maemura K, et al. Asymptomatic somatostatinoma of the pancreatic head: report of a case. Surg Today. 2010; 40:569–573. PMID: 20496141.
Article5. Yu RS, Chen Y, Wang LH, Xu XF, Jiang DY. A large functional somatostatinoma in the pancreatic tail: atypical CT appearances. Turk J Gastroenterol. 2009; 20:291–294. PMID: 20084576.
Article6. Williamson JM, Thorn CC, Spalding D, Williamson RC. Pancreatic and peripancreatic somatostatinomas. Ann R Coll Surg Engl. 2011; 93:356–360. PMID: 21943457.
Article7. Zhang B, Xie QP, Gao SL, Fu YB, Wu YL. Pancreatic somatostatinoma with obscure inhibitory syndrome and mixed pathological pattern. J Zhejiang Univ Sci B. 2010; 11:22–26. PMID: 20043348.
Article8. Cao XP, Liu YY, Xiao HP, Li YB, Wang LT, Xiao P. Pancreatic somatostatinoma characterized by extreme hypoglycemia. Chin Med J (Engl). 2009; 122:1709–1712. PMID: 19719976.9. Colović RB, Matić SV, Micev MT, Grubor NM, Atkinson HD, Latincić SM. Two synchronous somatostatinomas of the duodenum and pancreatic head in one patient. World J Gastroenterol. 2009; 15:5859–5863. PMID: 19998510.10. Musumba CO, Usman-Saeed M, O'Toole P, Powell S, Smart HL. Persistent severe gastrointestinal bleeding in a man with metastatic somatostatinoma. Gut. 2012; 61:277–328. PMID: 21940726.
Article11. Saifuddin T, Linder C, Banerjee B. Duodenal somatostatinoma presenting as upper gastrointestinal bleeding. Am J Gastroenterol. 1999; 94:1405–1408. PMID: 10235228.
Article12. Rios A, Fernandez JA, Rodríguez JM, Lujan JA, Martínez E, Parrilla P. Massive upper gastrointestinal bleeding as a manifestation of somatostatinoma of the ampulla of vater. Dig Dis Sci. 2001; 46:2162–2165. PMID: 11680591.13. Prachayakul V, Aswakul P, Pongprasobchai S, et al. Clinical characteristics, endosonographic findings and etiologies of gastroduodenal subepithelial lesions: a Thai referral single center study. J Med Assoc Thai. 2012; 95(Suppl 2):S61–S67. PMID: 22574531.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Gastric Carcinoid Tumor with Massive Bleeding).
- Mature Cystic Gastric Teratoma in an Infant: A Case Presenting with a Gastrointestinal Bleeding
- Endoscopic Hemoclipping Treatment for Gastric Dieulafoy Lesion in a Newborn
- A Case of a Y-shaped Pedunculated Gastric Polyp Presenting as an Upper Gastrointestinal Bleeding in a Patient with Chronic Renal Failure
- Combined Upper Gastrointestinal Lesions with Esophageal Varices