Clin Endosc.
2013 Sep;46(5):563-567.
Duodenal Mucosa-Associated Lymphoid Tissue Lymphomas: Two Cases and the Evaluation of Endoscopic Ultrasonography
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Yangsan, Korea. mdkhwook@gmail.com
Abstract
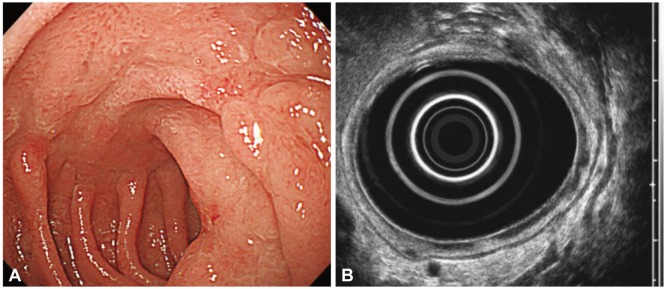
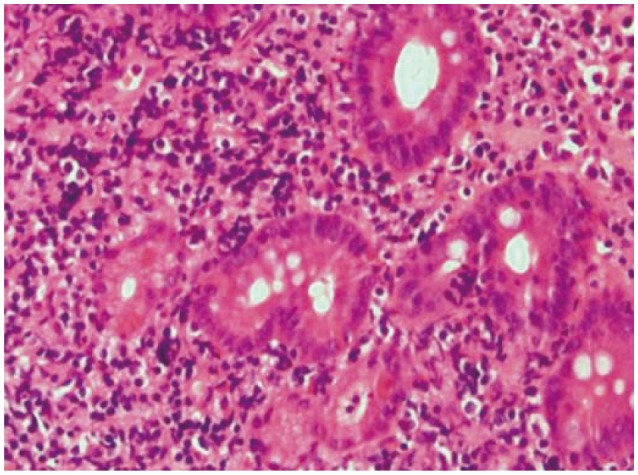
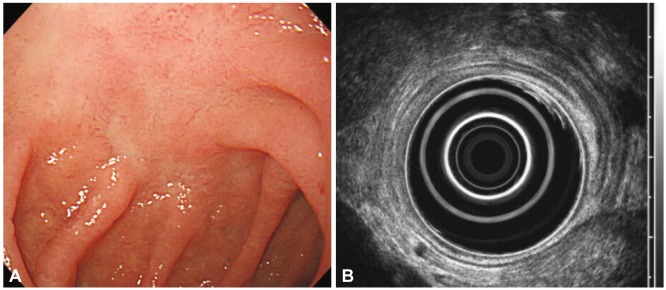
- Mucosa-associated lymphoid tissue lymphoma mainly arises in the stomach, with fewer than 30% arising in the small intestine. We describe here two cases of primary duodenal mucosa-associated lymphoid tissue lymphoma which were evaluated by endoscopic ultrasonography. A 52-year-old man underwent endoscopy due to abdominal pain, which demonstrated a depressed lesion on duodenal bulb. Endoscopic ultrasonographic finding was hypoechoic lesion invading the submucosa. The other case was a previously healthy 51-year-old man. Endoscopy showed a whitish granular lesion on duodenum third portion. Endoscopic ultrasonography image was similar to the first case, whereas abdominal computed tomography revealed enlargement of multiple lymph nodes. The first case was treated with eradication of Helicobacter pylori, after which the mucosal change and endoscopic ultrasound finding were normalized in 7 months. The second case was treated with cyclophosphamide, vincristine, prednisolone, and rituximab every 3 weeks. After 6 courses of chemotherapy, the patient achieved complete remission.
Keyword
MeSH Terms
-
Abdominal Pain
Antibodies, Monoclonal, Murine-Derived
Cyclophosphamide
Duodenum
Endoscopy
Endosonography
Helicobacter pylori
Humans
Intestine, Small
Lymph Nodes
Lymphoid Tissue
Lymphoma, B-Cell, Marginal Zone
Middle Aged
Prednisolone
Stomach
Vincristine
Rituximab
Antibodies, Monoclonal, Murine-Derived
Cyclophosphamide
Prednisolone
Vincristine
Figure
Reference
-
1. Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue: a distinctive type of B-cell lymphoma. Cancer. 1983; 52:1410–1416. PMID: 6193858.
Article2. Isaacson P, Chott A, Nakamura S, et al. Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymph oma). In : Swerdlow SH, Campo E, Harris NL, editors. WHO Classifi cation of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: In ternational Agency for Research on Cancer;2008. p. 214–217.3. Song IS, Choi KW, Kim CY, et al. Clinicopathologic study of primary gastric lymphoma of B-cell lymphoma of MALT. Korean J Gastroenterol. 1998; 31:463–476.4. Yokoi T, Nakamura T, Nakamura S. Differential diagnosis of the superficial-type gastric malignant lymphoma: differential diagnosis of gastric MALT lymphomas. Stomach Intest. 2001; 36:13–20.5. Mehra M, Agarwal B. Endoscopic diagnosis and staging of mucosa-associated lymphoid tissue lymphoma. Curr Opin Gastroenterol. 2008; 24:623–626. PMID: 19122505.
Article6. Suekane H, Iida M, Yao T, Matsumoto T, Masuda Y, Fujishima M. Endoscopic ultrasonography in primary gastric lymphoma: correlation with endoscopic and histologic findings. Gastrointest Endosc. 1993; 39:139–145. PMID: 8495833.
Article7. Caletti G, Fusaroli P, Togliani T. EUS in MALT lymphoma. Gastrointest Endosc. 2002; 56(4 Suppl):S21–S26. PMID: 12297744.
Article8. Nakamura S, Matsumoto T, Suekane H, et al. Predictive value of endoscopic ultrasonography for regression of gastric low grade and high grade MALT lymphomas after eradication of Helicobacter pylori. Gut. 2001; 48:454–460. PMID: 11247887.
Article9. El-Zahabi LM, Jamali FR, El-Hajj II, et al. The value of EUS in predicting the response of gastric mucosa-associated lymphoid tissue lymphoma to Helicobacter pylori eradication. Gastrointest Endosc. 2007; 65:89–96. PMID: 17185085.
Article10. Nagashima R, Takeda H, Maeda K, Ohno S, Takahashi T. Regression of duodenal mucosa-associated lymphoid tissue lymphoma after eradication of Helicobacter pylori. Gastroenterology. 1996; 111:1674–1678. PMID: 8942749.
Article11. Kamura M, Matsui K, Kokubo Y, et al. A case of the mucosa-associated lymphoid tissue lymphoma in the duodenal bulb improved rapidly by eradication of Helicobacter pylori for 4-years. Gastroenterol Endosc. 2000; 42:164–168.12. Kim JS, Jung HC, Shin KH, Song IS, Kim CW, Kim CY. Eradication of Helicobacter pylori infection did not lead to cure of duodenal mucosa-associated lymphoid tissue lymphoma. Scand J Gastroenterol. 1999; 34:215–218. PMID: 10192204.13. Fukazawa K, Sato K, Kihira K, et al. A cese of duodenal low-grade mucosa-associated lymphoid tissue lymphoma which did not respond to eradication therapy for Helicobacter pylori infection. Gastroenterol Endosc. 1999; 41:1484–1489.14. Xiang Z, Onoda N, Ohira M, et al. Mucosa-associated lymphoid tissue lymphoma of the duodenum: report of a case resistant to Helicobacter pylori eradication. Hepatogastroenterology. 2004; 51:732–735. PMID: 15143903.15. Woo KH, Kim JH, Yoon SB, et al. Duodenal mucosa-associated lymphoid tissue lymphoma: a case report. Korean J Intern Med. 2007; 22:296–299. PMID: 18309692.
Article16. Bertoni F, Coiffier B, Salles G, et al. MALT lymphomas: pathogenesis can drive treatment. Oncology (Williston Park). 2011; 25:1134–1142. 1147PMID: 22229204.17. Ruskoné-Fourmestraux A, Lavergne A, Aegerter PH, et al. Predictive factors for regression of gastric MALT lymphoma after anti-Helicobacter pylori treatment. Gut. 2001; 48:297–303. PMID: 11171816.18. Choi MK, Kim GH. Diagnosis and treatment of gastric MALT lymphoma. Korean J Gastroenterol. 2011; 57:272–280. PMID: 21623135.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Helicobacter pylori-negative Gastric Mucosa-associated Lymphoid Tissue Lymphoma
- Primary Esophageal Mucosa-associated Lymphoid Tissue Lymphoma: A Rare Case Report and Review of Other Published Data
- Duodenal Mucosa-associated Lymphoid Tissue Lymphoma Treated with Chemotherapy
- Primary Duodenal Mucosa-associated Lymphoid Tissue Lymphoma Treated with Radiation Therapy Alone
- A Case of Duodenal Mucosa-associated Lymphoid Tissue Lymphoma Presenting as a Refractory Ulcer