Clin Endosc.
2014 Jan;47(1):31-39.
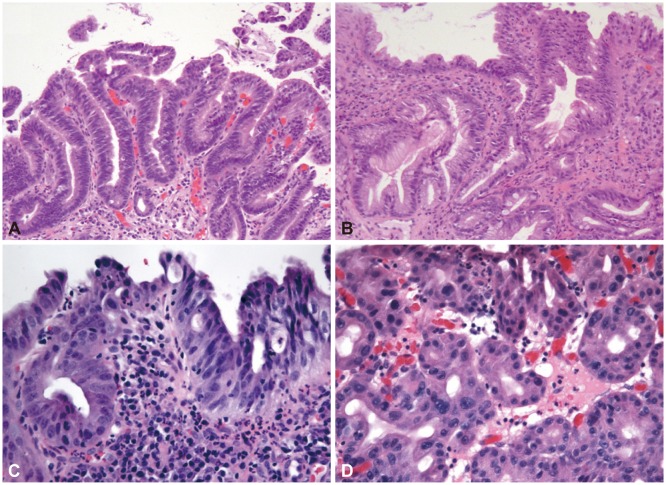
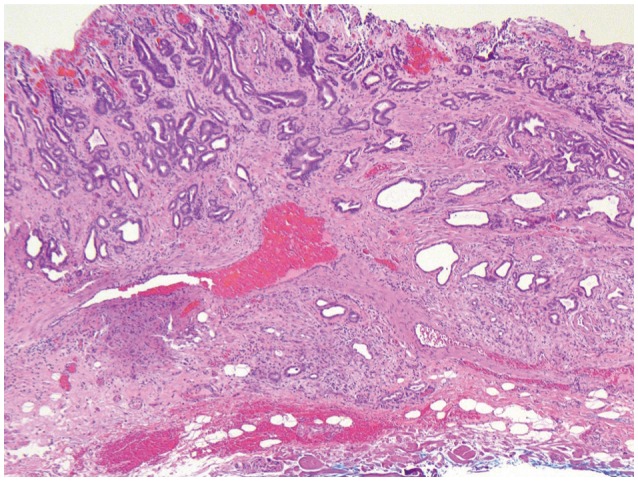
Histopathology in Barrett Esophagus and Barrett Esophagus-Related Dysplasia
- Affiliations
-
- 1Division of Pathology, Department of Laboratory Medicine, The Li Ka Shing Knowledge Institute, St. Michael's Hospital, the University of Toronto Faculty of Medicine, Toronto, ON, Canada. streutkerc@smh.ca
Abstract
- Pathologic specimens, both biopsies and endoscopic mucosal resections, for Barrett esophagus and Barrett-associated dysplasia and malignancy are common for pathologists in North America, and the incidence in South Asian countries seems to be increasing. Dysplasia and malignancy arising in intestinalized gastric-type mucosa raises issues in the interpretation of dysplasia and the evaluation of the depth of invasion of malignancies that are not seen in squamous dysplasia and squamous cell carcinoma. We review the North American approach to these lesions.
MeSH Terms
Figure
Reference
-
1. de Jonge PJ, van Blankenstein M, Grady WM, Kuipers EJ. Barrett's oesophagus: epidemiology, cancer risk and implications for management. Gut. 2014; 63:191–202. PMID: 24092861.
Article2. Ishimura N, Amano Y, Sollano JD, et al. Questionnaire-based survey conducted in 2011 concerning endoscopic management of Barrett's esophagus in East Asian countries. Digestion. 2012; 86:136–146. PMID: 22846450.
Article3. Wang KK, Sampliner RE. Practice Parameters Committee of the American College of Gastroenterology. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus. Am J Gastroenterol. 2008; 103:788–797. PMID: 18341497.
Article4. American Gastroenterological Association. Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association medical position statement on the management of Barrett's esophagus. Gastroenterology. 2011; 140:1084–1091. PMID: 21376940.
Article5. Ogiya K, Kawano T, Ito E, et al. Lower esophageal palisade vessels and the definition of Barrett's esophagus. Dis Esophagus. 2008; 21:645–649. PMID: 18459993.
Article6. Playford RJ. New British Society of Gastroenterology (BSG) guidelines for the diagnosis and management of Barrett's oesophagus. Gut. 2006; 55:442. PMID: 16531521.
Article7. Fitzgerald RC, di Pietro M, Ragunath K, et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett's oesophagus. Gut. 2014; 63:7–42. PMID: 24165758.
Article8. Harrison R, Perry I, Haddadin W, et al. Detection of intestinal metaplasia in Barrett's esophagus: an observational comparator study suggests the need for a minimum of eight biopsies. Am J Gastroenterol. 2007; 102:1154–1161. PMID: 17433019.
Article9. Gatenby PA, Ramus JR, Caygill CP, Shepherd NA, Watson A. Relevance of the detection of intestinal metaplasia in non-dysplastic columnar-lined oesophagus. Scand J Gastroenterol. 2008; 43:524–530. PMID: 18415743.
Article10. Liu W, Hahn H, Odze RD, Goyal RK. Metaplastic esophageal columnar epithelium without goblet cells shows DNA content abnormalities similar to goblet cell-containing epithelium. Am J Gastroenterol. 2009; 104:816–824. PMID: 19293780.
Article11. Hahn HP, Blount PL, Ayub K, et al. Intestinal differentiation in metaplastic, nongoblet columnar epithelium in the esophagus. Am J Surg Pathol. 2009; 33:1006–1015. PMID: 19363439.
Article12. Chaves P, Cruz C, Dias Pereira A, et al. Gastric and intestinal differentiation in Barrett's metaplasia and associated adenocarcinoma. Dis Esophagus. 2005; 18:383–387. PMID: 16336609.
Article13. Takubo K, Aida J, Naomoto Y, et al. Cardiac rather than intestinal-type background in endoscopic resection specimens of minute Barrett adenocarcinoma. Hum Pathol. 2009; 40:65–74. PMID: 18755496.
Article14. Kelty CJ, Gough MD, Van Wyk Q, Stephenson TJ, Ackroyd R. Barrett's oesophagus: intestinal metaplasia is not essential for cancer risk. Scand J Gastroenterol. 2007; 42:1271–1274. PMID: 17852872.
Article15. Chandrasoma P, Wijetunge S, DeMeester S, et al. Columnar-lined esophagus without intestinal metaplasia has no proven risk of adenocarcinoma. Am J Surg Pathol. 2012; 36:1–7. PMID: 21959311.
Article16. Westerhoff M, Hovan L, Lee C, Hart J. Effects of dropping the requirement for goblet cells from the diagnosis of Barrett's esophagus. Clin Gastroenterol Hepatol. 2012; 10:1232–1236. PMID: 22642957.
Article17. Srivastava A, Odze RD, Lauwers GY, Redston M, Antonioli DA, Glickman JN. Morphologic features are useful in distinguishing Barrett esophagus from carditis with intestinal metaplasia. Am J Surg Pathol. 2007; 31:1733–1741. PMID: 18059231.
Article18. Glickman JN, Fox V, Antonioli DA, Wang HH, Odze RD. Morphology of the cardia and significance of carditis in pediatric patients. Am J Surg Pathol. 2002; 26:1032–1039. PMID: 12170090.
Article19. Takubo K, Nixon JM, Jass JR. Ducts of esophageal glands proper and paneth cells in Barrett's esophagus: frequency in biopsy specimens. Pathology. 1995; 27:315–317. PMID: 8771147.
Article20. Riddell RH, Odze RD. Definition of Barrett's esophagus: time for a rethink: is intestinal metaplasia dead? Am J Gastroenterol. 2009; 104:2588–2594. PMID: 19623166.21. Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000; 47:251–255. PMID: 10896917.
Article22. Downs-Kelly E, Mendelin JE, Bennett AE, et al. Poor interobserver agreement in the distinction of high-grade dysplasia and adenocarcinoma in pretreatment Barrett's esophagus biopsies. Am J Gastroenterol. 2008; 103:2333–2340. PMID: 18671819.
Article23. Takubo K, Vieth M, Aida J, et al. Histopathological diagnosis of adenocarcinoma in Barrett's esophagus. Dig Endosc. Epub 2013 Aug 25. DOI: 10.1111/den.12160.24. Skacel M, Petras RE, Gramlich TL, Sigel JE, Richter JE, Goldblum JR. The diagnosis of low-grade dysplasia in Barrett's esophagus and its implications for disease progression. Am J Gastroenterol. 2000; 95:3383–3387. PMID: 11151865.
Article25. Curvers WL, ten Kate FJ, Krishnadath KK, et al. Low-grade dysplasia in Barrett's esophagus: overdiagnosed and underestimated. Am J Gastroenterol. 2010; 105:1523–1530. PMID: 20461069.
Article26. Lomo LC, Blount PL, Sanchez CA, et al. Crypt dysplasia with surface maturation: a clinical, pathologic, and molecular study of a Barrett's esophagus cohort. Am J Surg Pathol. 2006; 30:423–435. PMID: 16625087.27. Coco DP, Goldblum JR, Hornick JL, et al. Interobserver variability in the diagnosis of crypt dysplasia in Barrett esophagus. Am J Surg Pathol. 2011; 35:45–54. PMID: 21164286.
Article28. Mahajan D, Bennett AE, Liu X, Bena J, Bronner MP. Grading of gastric foveolar-type dysplasia in Barrett's esophagus. Mod Pathol. 2010; 23:1–11. PMID: 19838164.
Article29. Patil DT, Bennett AE, Mahajan D, Bronner MP. Distinguishing Barrett gastric foveolar dysplasia from reactive cardiac mucosa in gastroesophageal reflux disease. Hum Pathol. 2013; 44:1146–1153. PMID: 23332925.
Article30. Zhu W, Appelman HD, Greenson JK, et al. A histologically defined subset of high-grade dysplasia in Barrett mucosa is predictive of associated carcinoma. Am J Clin Pathol. 2009; 132:94–100. PMID: 19864239.
Article31. Patil DT, Goldblum JR, Rybicki L, et al. Prediction of adenocarcinoma in esophagectomy specimens based upon analysis of preresection biopsies of Barrett esophagus with at least high-grade dysplasia: a comparison of 2 systems. Am J Surg Pathol. 2012; 36:134–141. PMID: 22067333.32. Varghese S, Lao-Sirieix P, Fitzgerald RC. Identification and clinical implementation of biomarkers for Barrett's esophagus. Gastroenterology. 2012; 142:435–441. PMID: 22266150.
Article33. Appelman HD, Streutker C, Vieth M, et al. The esophageal mucosa and submucosa: immunohistology in GERD and Barrett's esophagus. Ann N Y Acad Sci. 2013; 1300:144–165. PMID: 24117640.
Article34. Kastelein F, Biermann K, Steyerberg EW, et al. Aberrant p53 protein expression is associated with an increased risk of neoplastic progression in patients with Barrett's oesophagus. Gut. 2013; 62:1676–1683. PMID: 23256952.
Article35. Kaye PV, Haider SA, Ilyas M, et al. Barrett's dysplasia and the Vienna classification: reproducibility, prediction of progression and impact of consensus reporting and p53 immunohistochemistry. Histopathology. 2009; 54:699–712. PMID: 19438745.
Article36. Kaye PV, Haider SA, James PD, et al. Novel staining pattern of p53 in Barrett's dysplasia: the absent pattern. Histopathology. 2010; 57:933–935. PMID: 21166706.37. Shi XY, Bhagwandeen B, Leong AS. p16, cyclin D1, Ki-67, and AMACR as markers for dysplasia in Barrett esophagus. Appl Immunohistochem Mol Morphol. 2008; 16:447–452. PMID: 18665038.
Article38. Dorer R, Odze RD. AMACR immunostaining is useful in detecting dysplastic epithelium in Barrett's esophagus, ulcerative colitis, and Crohn's disease. Am J Surg Pathol. 2006; 30:871–877. PMID: 16819330.
Article39. Scheil-Bertram S, Lorenz D, Ell C, Sheremet E, Fisseler-Eckhoff A. Expression of alpha-methylacyl coenzyme A racemase in the dysplasia carcinoma sequence associated with Barrett's esophagus. Mod Pathol. 2008; 21:961–967. PMID: 18500268.40. Lisovsky M, Falkowski O, Bhuiya T. Expression of alpha-methylacyl-coenzyme A racemase in dysplastic Barrett's epithelium. Hum Pathol. 2006; 37:1601–1606. PMID: 16996568.41. Kastelein F, Biermann K, Steyerberg EW, et al. Value of alpha-methylacyl-CoA racemase immunochemistry for predicting neoplastic progression in Barrett's oesophagus. Histopathology. 2013; 63:630–639. PMID: 24004067.42. Sonwalkar SA, Rotimi O, Scott N, et al. A study of indefinite for dysplasia in Barrett's oesophagus: reproducibility of diagnosis, clinical outcomes and predicting progression with AMACR (alpha-methylacyl-CoA-racemase). Histopathology. 2010; 56:900–907. PMID: 20636793.43. Lewis CJ, Thrumurthy SG, Pritchard S, Armstrong G, Attwood SE. Comparison of COX-2, Ki-67, and BCL-2 expression in normal esophageal mucosa, Barrett's esophagus, dysplasia, and adenocarcinoma with postablation mucosa and implications for ablative therapies. Surg Endosc. 2011; 25:2564–2569. PMID: 21359892.
Article44. Prasad GA, Wang KK, Halling KC, et al. Utility of biomarkers in prediction of response to ablative therapy in Barrett's esophagus. Gastroenterology. 2008; 135:370–379. PMID: 18538141.
Article45. Ong CA, Shapiro J, Nason KS, et al. Three-gene immunohistochemical panel adds to clinical staging algorithms to predict prognosis for patients with esophageal adenocarcinoma. J Clin Oncol. 2013; 31:1576–1582. PMID: 23509313.
Article46. Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010; 376:687–697. PMID: 20728210.
Article47. Rubio CA, Riddell R. Musculo-fibrous anomaly in Barrett's mucosa with dysplasia. Am J Surg Pathol. 1988; 12:885–889. PMID: 3189695.
Article48. Takubo K, Sasajima K, Yamashita K, Tanaka Y, Fujita K. Double muscularis mucosae in Barrett's esophagus. Hum Pathol. 1991; 22:1158–1161. PMID: 1743701.
Article49. Nishimaki T, Hölscher AH, Schüler M, Becker K, Muto T, Siewert JR. Chronic esophagitis and subsequent morphological changes of the esophageal mucosa in Barrett's esophagus: a histological study of esophagectomy specimens. Surg Today. 1994; 24:203–209. PMID: 8003861.50. Barbour AP, Jones M, Brown I, et al. Risk stratification for early esophageal adenocarcinoma: analysis of lymphatic spread and prognostic factors. Ann Surg Oncol. 2010; 17:2494–2502. PMID: 20349213.
Article51. Abraham SC, Krasinskas AM, Correa AM, et al. Duplication of the muscularis mucosae in Barrett esophagus: an underrecognized feature and its implication for staging of adenocarcinoma. Am J Surg Pathol. 2007; 31:1719–1725. PMID: 18059229.
Article52. Kaneshiro DK, Post JC, Rybicki L, Rice TW, Goldblum JR. Clinical significance of the duplicated muscularis mucosae in Barrett esophagus-related superficial adenocarcinoma. Am J Surg Pathol. 2011; 35:697–700. PMID: 21490446.
Article53. Mandal RV, Forcione DG, Brugge WR, Nishioka NS, Mino-Kenudson M, Lauwers GY. Effect of tumor characteristics and duplication of the muscularis mucosae on the endoscopic staging of superficial Barrett esophagus-related neoplasia. Am J Surg Pathol. 2009; 33:620–625. PMID: 19047893.
Article54. Lewis JT, Wang KK, Abraham SC. Muscularis mucosae duplication and the musculo-fibrous anomaly in endoscopic mucosal resections for barrett esophagus: implications for staging of adenocarcinoma. Am J Surg Pathol. 2008; 32:566–571. PMID: 18300796.55. Hahn HP, Shahsafaei A, Odze RD. Vascular and lymphatic properties of the superficial and deep lamina propria in Barrett esophagus. Am J Surg Pathol. 2008; 32:1454–1461. PMID: 18685488.
Article56. Estrella JS, Hofstetter WL, Correa AM, et al. Duplicated muscularis mucosae invasion has similar risk of lymph node metastasis and recurrence-free survival as intramucosal esophageal adenocarcinoma. Am J Surg Pathol. 2011; 35:1045–1053. PMID: 21602659.
Article57. Vieth M, Stolte M. Pathology of early upper GI cancers. Best Pract Res Clin Gastroenterol. 2005; 19:857–869. PMID: 16338646.
Article58. Larghi A, Lightdale CJ, Ross AS, et al. Long-term follow-up of complete Barrett's eradication endoscopic mucosal resection (CBE-EMR) for the treatment of high grade dysplasia and intramucosal carcinoma. Endoscopy. 2007; 39:1086–1091. PMID: 17701854.
Article59. Manner H, Pech O, Heldmann Y, et al. Efficacy, safety, and long-term results of endoscopic treatment for early stage adenocarcinoma of the esophagus with low-risk sm1 invasion. Clin Gastroenterol Hepatol. 2013; 11:630–635. PMID: 23357492.
Article60. Lee JH, Kim JH, Choi JW, Kim YS. The presence of a micropapillary component predicts aggressive behaviour in early and advanced gastric adenocarcinomas. Pathology. 2010; 42:560–563. PMID: 20854075.
Article61. Eom DW, Kang GH, Han SH, et al. Gastric micropapillary carcinoma: a distinct subtype with a significantly worse prognosis in TNM stages I and II. Am J Surg Pathol. 2011; 35:84–91. PMID: 21164291.