Ann Dermatol.
2016 Jun;28(3):375-380. 10.5021/ad.2016.28.3.375.
Tumoral Calcinosis as an Initial Complaint of Juvenile-Onset Amyopathic Dermatomyositis
- Affiliations
-
- 1Department of Dermatology, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea. sycho@snu.ac.kr
- 2Department of Laboratory Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2164647
- DOI: http://doi.org/10.5021/ad.2016.28.3.375
Abstract
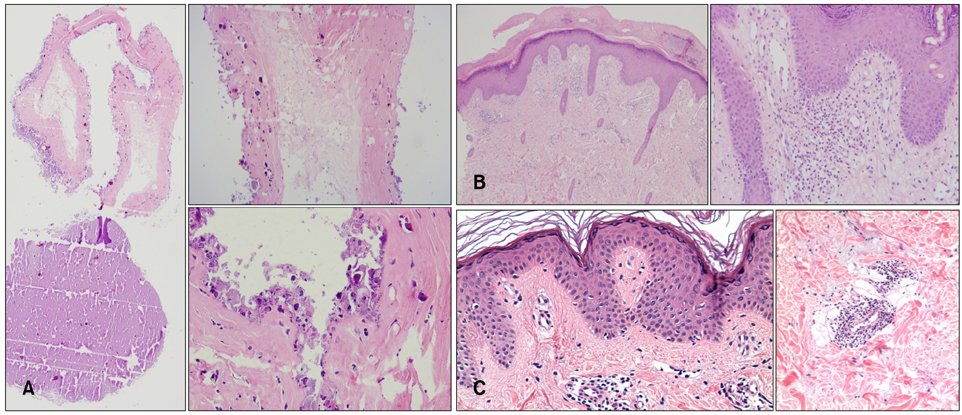
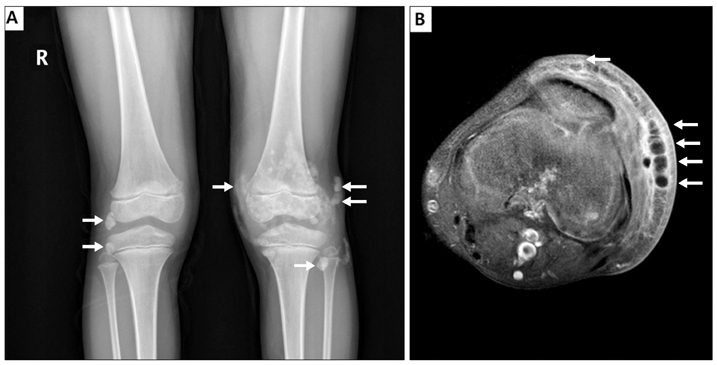
- Calcinosis is rarely observed in juvenile-onset amyopathic dermatomyositis in contrast to juvenile-onset dermatomyositis. A 6-year-old female presented with several 0.5 to 2 cm-sized painless grouped masses on both knees for 3 years. The patient also presented with multiple erythematous scaly patches and plaques on both elbows, knuckles, buttock, ankles and cheeks. Her mother had similar skin lesions which were erythematous scaly patches on the knuckles and elbows, since her childhood. When skin biopsy was performed from a left knee nodule, liquid chalky discharge was observed. The biopsy results were consistent with calcinosis cutis. Other biopsies from erythematous patch of the patient and erythematous patch of her mother showed vacuolization of basal cell layer with inflammatory cell infiltrations. Laboratory findings showed normal range of serum phosphorus (4.5 mg/dl), calcium (9.3 mg/dl), 1,25-dihydroxy-vitamin D (10.8 ng/ml) and parathyroid hormone levels (11 pg/ml). Both patient and her mother had no history of muscle weakness and showed normal levels of muscle-specific enzyme. Both patients were diagnosed with juvenile-onset amyopathic dermatomyositis based on histopathology and cutaneous manifestations with no evidence of muscle weakness and no serum muscle enzyme abnormalities. Tumoral calcium deposits observed in daughter was diagnosed as dystrophic calcinosis which can be rarely seen in juvenile-onset amyopathic dermatomyositis. The patient is being treated with oral acetazolamide (40 mg/kg/d) for calcinosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Reiter N, El-Shabrawi L, Leinweber B, Berghold A, Aberer E. Calcinosis cutis: part I. Diagnostic pathway. J Am Acad Dermatol. 2011; 65:1–12. quiz 13-14.2. Balcı DD, Celik E, Sarikaya G, Yenin JZ, Atik E. The co-existence of vulvar lichen sclerosus, ulcerated calcinosis cutis, and dermatomyositis: coincidence or immunological mechanism. Ann Dermatol. 2011; 23:Suppl 3. S375–S379.
Article3. Balin SJ, Wetter DA, Andersen LK, Davis MD. Calcinosis cutis occurring in association with autoimmune connective tissue disease: the mayo clinic experience with 78 patients, 1996-2009. Arch Dermatol. 2012; 148:455–462.
Article4. Gerami P, Walling HW, Lewis J, Doughty L, Sontheimer RD. A systematic review of juvenile-onset clinically amyopathic dermatomyositis. Br J Dermatol. 2007; 157:637–644.
Article5. Walling HW, Gerami P, Sontheimer RD. Juvenile-onset clinically amyopathic dermatomyositis: an overview of recent progress in diagnosis and management. Paediatr Drugs. 2010; 12:23–34.6. Gowdie PJ, Allen RC, Kornberg AJ, Akikusa JD. Clinical features and disease course of patients with juvenile dermatomyositis. Int J Rheum Dis. 2013; 16:561–567.
Article7. Samson C, Soulen RL, Gursel E. Milk of calcium fluid collections in juvenile dermatomyositis: MR characteristics. Pediatr Radiol. 2000; 30:28–29.
Article8. Jiang X, Yi Q, Liu D, Wang S, Li L. A case of juvenile dermatomyositis with severe calcinosis and successful treatment with prednisone and diltiazem. Int J Dermatol. 2011; 50:74–77.
Article9. Mukamel M, Horev G, Mimouni M. New insight into calcinosis of juvenile dermatomyositis: a study of composition and treatment. J Pediatr. 2001; 138:763–766.
Article10. Oliveri MB, Palermo R, Mautalen C, Hübscher O. Regression of calcinosis during diltiazem treatment in juvenile dermatomyositis. J Rheumatol. 1996; 23:2152–2155.11. Ichiki Y, Akiyama T, Shimozawa N, Suzuki Y, Kondo N, Kitajima Y. An extremely severe case of cutaneous calcinosis with juvenile dermatomyositis, and successful treatment with diltiazem. Br J Dermatol. 2001; 144:894–897.
Article12. Shimizu M, Ueno K, Ishikawa S, Yokoyama T, Kasahara Y, Yachie A. Cutaneous calcinosis in juvenile dermatomyositis. J Pediatr. 2013; 163:921.
Article13. Hoeltzel MF, Oberle EJ, Robinson AB, Agarwal A, Rider LG. The presentation, assessment, pathogenesis, and treatment of calcinosis in juvenile dermatomyositis. Curr Rheumatol Rep. 2014; 16:467.
Article14. De Castro TC, Guarniero R, Giacomin MF, Meneghin MB, Martins GB, Lotufo Sde A. "Milk of calcium": a rare presentation of calcinosis. Rev Bras Reumatol. 2014; 54:65–67.15. Sprecher E. Familial tumoral calcinosis: from characterization of a rare phenotype to the pathogenesis of ectopic calcification. J Invest Dermatol. 2010; 130:652–660.
Article16. Hershkovitz D, Gross Y, Nahum S, Yehezkel S, Sarig O, Uitto J, et al. Functional characterization of SAMD9, a protein deficient in normophosphatemic familial tumoral calcinosis. J Invest Dermatol. 2011; 131:662–669.
Article17. Shimizu M, Ueno K, Ishikawa S, Kasahara Y, Yachie A. Role of activated macrophage and inflammatory cytokines in the development of calcinosis in juvenile dermatomyositis. Rheumatology (Oxford). 2014; 53:766–767.
Article18. Peñate Y, Guillermo N, Melwani P, Martel R, Hernández-Machín B, Borrego L. Calcinosis cutis associated with amyopathic dermatomyositis: response to intravenous immunoglobulin. J Am Acad Dermatol. 2009; 60:1076–1077.
Article19. Lammoglia JJ, Mericq V. Familial tumoral calcinosis caused by a novel FGF23 mutation: response to induction of tubular renal acidosis with acetazolamide and the non-calcium phosphate binder sevelamer. Horm Res. 2009; 71:178–184.
Article20. Marie I, Ménard JF, Hachulla E, Chérin P, Benveniste O, Tiev K, et al. Infectious complications in polymyositis and dermatomyositis: a series of 279 patients. Semin Arthritis Rheum. 2011; 41:48–60.
Article