Clinical Outcome of Remnant Thyroid Ablation with Low Dose Radioiodine in Korean Patients with Low to Intermediate-risk Thyroid Cancer
- Affiliations
-
- 1Department of Nuclear Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Nuclear Medicine, Seoul National University Boramae Medical Center, Seoul, Korea. mdosw@snu.ac.kr
- 3Department of Surgery, Seoul National University Boramae Medical Center, Seoul, Korea.
- 4Department of Otolaryngology, Seoul National University Boramae Medical Center, Seoul, Korea.
- 5Department of Internal Medicine, Seoul National University Boramae Medical Center, Seoul, Korea.
- 6Department of Biomedical Sciences, Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 7Laboratory of Molecular Imaging and Therapy, Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 8Tumor Microenvironment Global Core Research Center, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2164471
- DOI: http://doi.org/10.3346/jkms.2015.30.7.876
Abstract
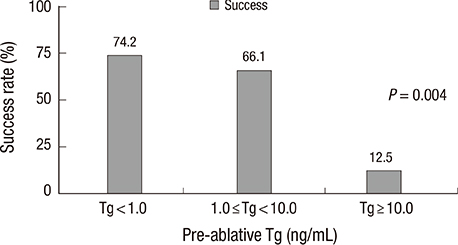
- Radioiodine activity required for remnant thyroid ablation is of great concern, to avoid unnecessary exposure to radiation and minimize adverse effects. We investigated clinical outcomes of remnant thyroid ablation with a low radioiodine activity in Korean patients with low to intermediate-risk thyroid cancer. For remnant thyroid ablation, 176 patients received radioiodine of 1.1 GBq, under a standard thyroid hormone withdrawal and a low iodine diet protocol. Serum levels of thyroid stimulating hormone stimulated thyroglobulin (off-Tg) and thyroglobulin-antibody (Tg-Ab), and a post-therapy whole body scan (RxWBS) were evaluated. Completion of remnant ablation was considered when there was no visible uptake on RxWBS and undetectable off-Tg (<1.0 ng/mL). Various factors including age, off-Tg, and histopathology were analyzed to predict ablation success rates. Of 176 patients, 68.8% (n = 121) who achieved successful remnant ablation were classified into Group A, and the remaining 55 were classified into Group B. Group A presented with significantly lower off-Tg at the first radioiodine administration (pre-ablative Tg) than those of Group B (1.2 +/- 2.3 ng/mL vs. 6.2 +/- 15.2 ng/mL, P = 0.027). Pre-ablative Tg was the only significant factor related with ablation success rates. Diagnostic performances of pre-ablative Tg < 10.0 ng/mL were sensitivity of 99.1%, specificity of 14.0%, positive predictive value of 71.1%, and negative predictive value of 87.5%, respectively. Single administration of low radioiodine activity could be sufficient for remnant thyroid ablation in patients with low to intermediate-risk thyroid cancer. Pre-ablative Tg with cutoff value of 10.0 ng/mL is a promising factor to predict successful remnant ablation.
MeSH Terms
Figure
Cited by 3 articles
-
Pathological N1b Node Metastasis Itself Can Be Still a Valid Prognostic Factor in PTC after High Dose RAI Therapy
Choon-Young Kim, Seung Hyun Son, Ji-hoon Jung, Chang-Hee Lee, Ju Hye Jeong, Shin Young Jeong, Sang-Woo Lee, Byeong-Cheol Ahn, Jaetae Lee
Int J Thyroidol. 2016;9(2):159-167. doi: 10.11106/ijt.2016.9.2.159.2016 Revised Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules and Thyroid Cancer
Ka Hee Yi, Eun Kyung Lee, Ho-Cheol Kang, Sun Wook Kim, In Joo Kim, So Yeon Park, Kee-Hyun Nam, Jin Woo Park, Sang Kyun Bae, Seung-Kuk Baek, Jung Hwan Baek, Byung-Joo Lee, Ki-Wook Chung, Yuh-Seog Jung, Gi Jeong Cheon, Won Bae Kim, Jae Hoon Chung, Young-Soo Rho, Dong Gyu Na, Yunwoo Koh
Int J Thyroidol. 2016;9(2):59-126. doi: 10.11106/ijt.2016.9.2.59.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 6. Radioactive Iodine Treatment after Thyroidectomy 2024
Sohyun Park, Ari Chong, Ho-Cheol Kang, Keunyoung Kim, Sun Wook Kim, Dong Gyu Na, Young Joo Park, Ji-In Bang, Youngduk Seo, Young Shin Song, So Won Oh, Eun Kyung Lee, Dong-Jun Lim, Yun Jae Chung, Chae Moon Hong, Sang-Woo Lee
Int J Thyroidol. 2024;17(1):97-110. doi: 10.11106/ijt.2024.17.1.97.
Reference
-
1. Sawka AM, Brierley JD, Tsang RW, Thabane L, Rotstein L, Gafni A, Straus S, Goldstein DP. An updated systematic review and commentary examining the effectiveness of radioactive iodine remnant ablation in well-differentiated thyroid cancer. Endocrinol Metab Clin North Am. 2008; 37:457–480. x2. Eustatia-Rutten CF, Smit JW, Romijn JA, van der Kleij-Corssmit EP, Pereira AM, Stokkel MP, Kievit J. Diagnostic value of serum thyroglobulin measurements in the follow-up of differentiated thyroid carcinoma, a structured meta-analysis. Clin Endocrinol (Oxf). 2004; 61:61–74.3. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.4. Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JW, Wiersinga W. European Thyroid Cancer Taskforce. European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol. 2006; 154:787–803.5. Schlumberger MJ. Papillary and follicular thyroid carcinoma. N Engl J Med. 1998; 338:297–306.6. Mazzaferri EL. Thyroid remnant 131I ablation for papillary and follicular thyroid carcinoma. Thyroid. 1997; 7:265–271.7. Doi SA, Woodhouse NJ. Ablation of the thyroid remnant and 131I dose in differentiated thyroid cancer. Clin Endocrinol (Oxf). 2000; 52:765–773.8. Hackshaw A, Harmer C, Mallick U, Haq M, Franklyn JA. 131I activity for remnant ablation in patients with differentiated thyroid cancer: A systematic review. J Clin Endocrinol Metab. 2007; 92:28–38.9. Cherk MH, Kalff V, Yap KS, Bailey M, Topliss D, Kelly MJ. Incidence of radiation thyroiditis and thyroid remnant ablation success rates following 1110 MBq (30 mCi) and 3700 MBq (100 mCi) post-surgical 131I ablation therapy for differentiated thyroid carcinoma. Clin Endocrinol (Oxf). 2008; 69:957–962.10. Mandel SJ, Mandel L. Radioactive iodine and the salivary glands. Thyroid. 2003; 13:265–271.11. Kloos RT, Duvuuri V, Jhiang SM, Cahill KV, Foster JA, Burns JA. Nasolacrimal drainage system obstruction from radioactive iodine therapy for thyroid carcinoma. J Clin Endocrinol Metab. 2002; 87:5817–5820.12. Mallick U, Harmer C, Yap B, Wadsley J, Clarke S, Moss L, Nicol A, Clark PM, Farnell K, McCready R, et al. Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med. 2012; 366:1674–1685.13. Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B, Bardet S, Leenhardt L, Bastie D, Schvartz C, et al. Tumeurs de la Thyroïde Refractaires Network for the Essai Stimulation Ablation Equivalence Trial. Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med. 2012; 366:1663–1673.14. Schlumberger M, Berg G, Cohen O, Duntas L, Jamar F, Jarzab B, Limbert E, Lind P, Pacini F, Reiners C, et al. Follow-up of low-risk patients with differentiated thyroid carcinoma: a European perspective. Eur J Endocrinol. 2004; 150:105–112.15. Pacini F, Capezzone M, Elisei R, Ceccarelli C, Taddei D, Pinchera A. Diagnostic 131-iodine whole-body scan may be avoided in thyroid cancer patients who have undetectable stimulated serum Tg levels after initial treatment. J Clin Endocrinol Metab. 2002; 87:1499–1501.16. Park EK, Chung JK, Lim IH, Park do J, Lee DS, Lee MC, Cho BY. Recurrent/metastatic thyroid carcinomas false negative for serum thyroglobulin but positive by posttherapy I-131 whole body scans. Eur J Nucl Med Mol Imaging. 2009; 36:172–179.17. Cho BY, Koh CS, Lee MC, Chung JK, Lee DS, Kim YK, Jeong JM. Ablation of remnant thyroid tissue with I-131 in well differentiated thyroid cancer after surgery. Korean J Nucl Med. 1997; 31:339–345.18. McDougall IR. The case for obtaining a diagnostic whole-body scan prior to iodine 131 treatment of differentiated thyroid cancer. Thyroid. 2009; 19:811–813.19. McDougall IR, Iagaru A. Thyroid stunning: fact or fiction? Semin Nucl Med. 2011; 41:105–112.20. Lee HJ, Rha SY, Jo YS, Kim SM, Ku BJ, Shong M, Kim YK, Ro HK. Predictive value of the preablation serum thyroglobulin level after thyroidectomy is combined with postablation 131I whole body scintigraphy for successful ablation in patients with differentiated thyroid carcinoma. Am J Clin Oncol. 2007; 30:63–68.21. Giovanella L, Ceriani L, Ghelfo A, Keller F. Thyroglobulin assay 4 weeks after thyroidectomy predicts outcome in low-risk papillary thyroid carcinoma. Clin Chem Lab Med. 2005; 43:843–847.22. Polachek A, Hirsch D, Tzvetov G, Grozinsky-Glasberg S, Slutski I, Singer J, Weinstein R, Shimon I, Benbassat CA. Prognostic value of post-thyroidectomy thyroglobulin levels in patients with differentiated thyroid cancer. J Endocrinol Invest. 2011; 34:855–860.23. Toubeau M, Touzery C, Arveux P, Chaplain G, Vaillant G, Berriolo A, Riedinger JM, Boichot C, Cochet A, Brunotte F. Predictive value for disease progression of serum thyroglobulin levels measured in the postoperative period and after (131)I ablation therapy in patients with differentiated thyroid cancer. J Nucl Med. 2004; 45:988–994.24. Webb RC, Howard RS, Stojadinovic A, Gaitonde DY, Wallace MK, Ahmed J, Burch HB. The utility of serum thyroglobulin measurement at the time of remnant ablation for predicting disease-free status in patients with differentiated thyroid cancer: a meta-analysis involving 3947 patients. J Clin Endocrinol Metab. 2012; 97:2754–2763.25. Vaisman A, Orlov S, Yip J, Hu C, Lim T, Dowar M, Freeman JL, Walfish PG. Application of post-surgical stimulated thyroglobulin for radioiodine remnant ablation selection in low-risk papillary thyroid carcinoma. Head Neck. 2010; 32:689–698.26. Rosario PW, Xavier AC, Calsolari MR. Value of postoperative thyroglobulin and ultrasonography for the indication of ablation and 131I activity in patients with thyroid cancer and low risk of recurrence. Thyroid. 2011; 21:49–53.27. Phan HT, Jager PL, van der Wal JE, Sluiter WJ, Plukker JT, Dierckx RA, Wolffenbuttel BH, Links TP. The follow-up of patients with differentiated thyroid cancer and undetectable thyroglobulin (Tg) and Tg antibodies during ablation. Eur J Endocrinol. 2008; 158:77–83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Low Dose versus High Dose Radioiodine Therapy
- Management guidelines for patients with thyroid cancer
- A Phase II Multi-Center, Non-Randomized, Parallel Group, Non-Inferiority Study to Compare the Efficacy of No Radioactive Iodine Remnant Ablation to Remnant Ablation Treatment in Low- to Intermediate-Risk of Papillary Thyroid Cancer: The MOREthyroid Trial Protocol
- Second Primary Malignancy after Radioiodine Treatment of Thyroid Disease: Current Status
- Diagnostic Whole-Body Scan May Not Be Necessary for Intermediate-Risk Patients with Differentiated Thyroid Cancer after Low-Dose (30 mCi) Radioactive Iodide Ablation