J Dent Rehabil Appl Sci.
2016 Mar;32(1):47-59. 10.14368/jdras.2016.32.1.47.
Changes in occlusal force depending on the movement of the adjacent and opposing teeth after loss of lower first molar: comparative study by using a strain gauge
- Affiliations
-
- 1Department of Orthodontics, Graduate School of Clinical Dentistry, Ewha Womans University, Seoul, Republic of Korea. yschun1000@gmail.com
- 2Department of Prosthodontics and Dental Research Institute, Seoul National University Gwanak Dental Hospital, Seoul, Republic of Korea.
- KMID: 2162379
- DOI: http://doi.org/10.14368/jdras.2016.32.1.47
Abstract
- PURPOSE
The aim of this study was to investigate the changes in occlusal force after loss of the lower first molar depending on the inclination and extrusion of the adjacent and opposing teeth by using a strain gauge.
MATERIALS AND METHODS
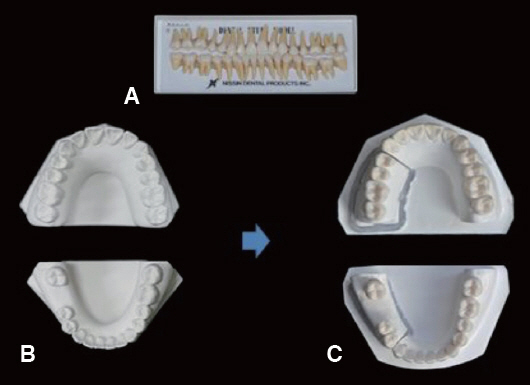
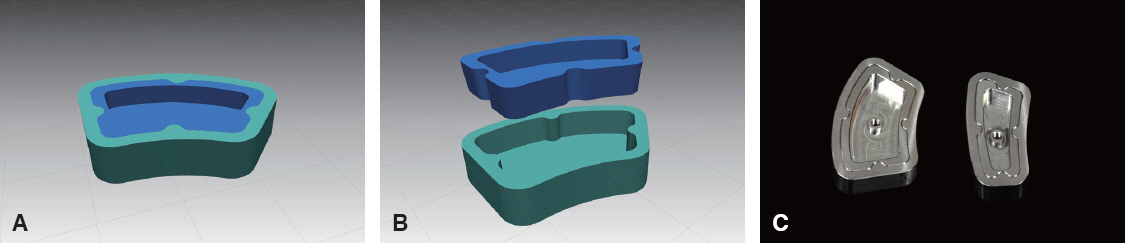
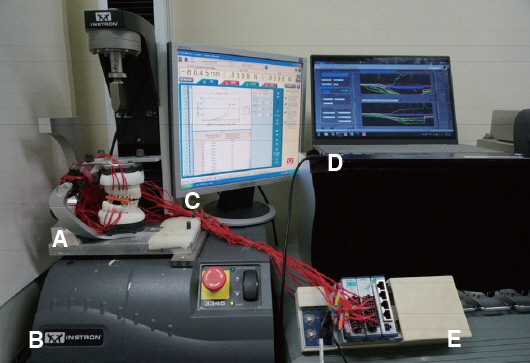
Anatomic teeth were used to reconstruct the normal dental arch with loss of the lower right first molar. A uniformly thick layer of silicone was applied to the root to mimic the periodontal ligament. Four stages of dies with varying degrees of inclination and extrusion of the adjacent and opposing teeth were constructed and attached to master model interchangeably by using a CAD/CAM fabricated customized die system. The strain gauges were attached to teeth and a universal testing machine was used to determine the changes in occlusal force. An independent t-test and one-way ANOVA were performed (α = .05).
RESULTS
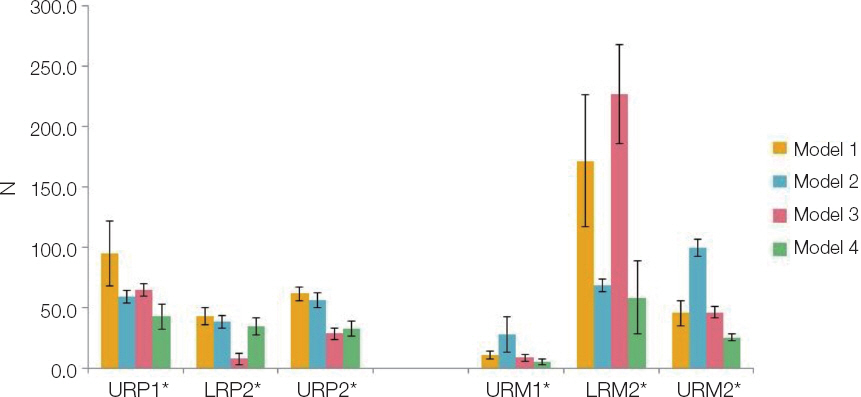
While simulating chewing food, the upper first, second premolar and lower second molar showed greater occlusal force than before extraction. When the change of adjacent teeth's occlusal force with their progressive movement after molar loss was evaluated, the difference among four die models was significant and was in the decreasing aspect (P < 0.05).
CONCLUSION
When the lower first molar was lost and the adjacent teeth did not move yet, the occlusal force in adjacent teeth was higher than that when the lower first molar still existed. In addition, the occlusal force in the upper premolars and lower second molar decreased significantly with the progressive movement of adjacent teeth.
MeSH Terms
Figure
Reference
-
References
1. Yalisove I, Deitz J. Telescopic prosthesis therapy. 1977. 1st ed. Philadelphia: George F. Strickly Co;p. 104–7.2. Stern N, Revah A, Becker A. The tilted posterior tooth. Part I: etiology, syndrome, and prevention. J Prosthet Dent. 1981; 46:404–7. DOI: 10.1016/0022-3913(81)90447-9.3. Craddock HL. Occlusal changes following posterior tooth loss in adults. Part 3. A study of clinical parameters associated with the presence of occlusal interferences following posterior tooth loss. J Prosthodont. 2008; 17:25–30. PMID: 17927736.4. Goldman HM, Cohen DW. Periodontal therapy. 1973. 5th ed. St. Louis: The C. V. Mosby Co;p. 40.5. Wehrbein H, Diedrich P. Mesio-marginal findings at tilted molars: a histological-histomorphometric study. Eur J Orthod. 2001; 23:663–70. DOI: 10.1093/ejo/23.6.663. PMID: 11890062.6. Yang HS, Thompson VP. A two-dimensional stress analysis comparing fixed prosthodontic approaches to the tilted molar abutment. Int J Prosthodont. 1991; 4:416–24. PMID: 1811637.7. Gibbs CH, Anusavice KJ, Young HM, Jones JS, Esquivel-Upshaw JF. Maximum clenching force of patients with moderate loss of posterior tooth support: a pilot study. J Prosthet Dent. 2002; 88:498–502. DOI: 10.1067/mpr.2002.129062. PMID: 12473999.8. Agerberg G, Carlsson GE. Chewing ability in relation to dental and general health: analysis of data obtained from a questionnaire. Acta Odontol Scand. 1981; 39:147–53. DOI: 10.3109/00016358109162273.9. Osterberg T, Steen B. Relationship between dental state and dietary intake in 70-year-old males and females in Göteborg, Sweden: a population study. J Oral Rehabil. 1982; 9:509–21. DOI: 10.1111/j.1365-2842.1982.tb01041.x. PMID: 6960162.10. Manly RS, Braley LC. Masticatory performance and efficiency. J Dent Res. 1950; 29:448–62. DOI: 10.1177/00220345500290040701.11. Devlin H, Wastell DG. Bite force and masseter muscle electromyographic activity during onset of an isometric clench in man. Arch Oral Biol. 1985; 30:213–5. DOI: 10.1016/0003-9969(85)90035-4.12. Fontijn-Tekamp FA, Slagter AP, Van der Bilt A, Van't Hof MA, Kalk W, Jansen JA. Swallowing thresholds of mandibular implant-retained overdentures with variable portion sizes. Clin Oral Implants Res. 2004; 15:375–80. DOI: 10.1111/j.1600-0501.2004.01006.x. PMID: 15142103.13. Helkimo E, Carlsson GE, Helkimo M. Bite force and state of dentition. Acta Odontol Scand. 1977; 35:297–303. DOI: 10.3109/00016357709064128. PMID: 271452.14. Tsuga K, Carlsson GE, Osterberg T, Karlsson S. Self-assessed masticatory ability in relation to maximal bite force and dental state in 80-year-old subjects. J Oral Rehabil. 1998; 25:117–24. DOI: 10.1046/j.1365-2842.1998.00233.x.15. Hemley S. Fundamentals of occlusion. 1944. 15th ed. Philadelphia: W.B. Saunders.16. Anderson DJ. Measurement of stress in mastication. II. J Dent Res. 1956; 35:671–3. DOI: 10.1177/00220345560350050301. DOI: 10.1177/00220345560350050201. PMID: 13367283.17. Fløystrand F, Kleven E, Oilo G. A novel miniature bite force recorder and its clinical application. Acta Odontol Scand. 1982; 40:209–14. DOI: 10.3109/00016358209019814. PMID: 6958166.18. Seo JC, Kim JR, Yang DK. Study on changes in the maximum bite force after orthognathic surgery. J Korean Assoc Oral Maxillofac Surg. 1996; 22:121–9.19. Cho YC, Kim TK. A study on maximum bite force after dental implantation. J Korean Assoc Oral Maxillofac Surg. 1997; 23:541–7.20. Jung BY, Jeon YS, Han DH. Occlusal force and oral tactile sensibility measured in partially edentulous patients with Brånemark implants and natural teeth: a clinical study. J Korean Acad Prosthodont. 1999; 37:23–41.21. Kwon HK, Yoo JH, Kwon YS, Kim BI. Comparison of bite force with dental prescale and unilateral bite force recorder in healthy subjects. J Korean Acad Prosthodont. 2006; 44:103–11.22. Maness W. Comparison of the duration of occlusal contacts during habitual closure using the digital occlusal senser [abstract]. J Dent Res. 1986; 65:141.23. Throckmorton GS, Rasmussen J, Caloss R. Calibration of T-scan sensors for recording bite forces in denture patients. J Oral Rehabil. 2009; 36:636–43. DOI: 10.1111/j.1365-2842.2009.01978.x. PMID: 19602099.24. Oyen OJ, Melugin MB, Indresano AT. Strain gauge analysis of the frontozygomatic region of the zygomatic complex. J Oral Maxillofac Surg. 1996; 54:1092–5. DOI: 10.1016/S0278-2391(96)90167-6.25. Kim SC, Park KC. An analytical study on strain distribution using strain gauge attached on root surface. Korean J Orthod. 2001; 31:325–33.26. Duyck J, Van Oosterwyck H, De Cooman M, Puers R, Vander Sloten J, Naert I. Three-dimensional force measurements on oral implants: a methodological study. J Oral Rehabil. 2000; 27:744–53. DOI: 10.1046/j.1365-2842.2000.00581.x. PMID: 11012848.27. Heo W, Baek SH. Friction properties according to vertical and horizontal tooth displacement and bracket type during inital leveling and alignment. Angle Orthod. 2011; 81:653–61. DOI: 10.2319/072310-431.1. PMID: 21306223.28. Sohn BS, Heo SJ, Chang IT, Koak JY, Kim SK. A strain gauge analysis of implant supported cantilevered fixed prosthesis under distal static load. J Korean Acad Prosthodont. 2007; 45:717–23.29. Pedersen E, Andersen K, Melse B. Tooth displacement analysed on human autopsy material by means of a strain gauge technique. Eur J Orthod. 1991; 13:65–74. DOI: 10.1093/ejo/13.1.65. PMID: 2032570.30. Gunne HS, Wall AK. The effect of new complete dentures on mastication and dietary intake. Acta Odontol Scand. 1985; 43:257–68. DOI: 10.3109/00016358509046506.31. Yurkstas A, Fridley HH, Manly RS. A functional evaluation of fixed and removable bridgework. J Prosthet Dent. 1951; 1:570–7. DOI: 10.1016/0022-3913(51)90042-X.32. Yurkstas AA. The effect of missing teeth on masticatory performance and efficiency. J Prosthet Dent. 1954; 4:120–3. DOI: 10.1016/0022-3913(54)90076-1.33. Lambrecht JR. The influence of occlusal contact area on chewing performance. J Prosthet Dent. 1965; 15:444–50. DOI: 10.1016/S0022-3913(65)80012-9.34. Iwase M, Ohashi M, Tachibana H, Toyoshima T, Nagumo M. Bite force, occlusal contact area and masticatory efficiency before and after orthognathic surgical correction of mandibular prognathism. Int J Oral Maxillofac Surg. 2006; 35:1102–7. DOI: 10.1016/j.ijom.2006.08.014. PMID: 17097270.35. Yoon HR, Choi YJ, Kim KH, Chung C. Comparisons of occlusal force according to occlusal relationship, skeletal pattern, age and gender in Koreans. Korean J Orthod. 2010; 40:304–313. DOI: 10.4041/kjod.2010.40.5.304.36. Korioth TW. Number and location of occlusal contacts in intercuspal position. J Prosthet Dent. 1990; 64:206–10. DOI: 10.1016/0022-3913(90)90180-K.37. Picton DC. Tilting movements of teeth during biting. Arch Oral Biol. 1962; 7:151–9. DOI: 10.1016/0003-9969(62)90003-1.38. Southard TE, Behrents RG, Tolley EA. The anterior component of occlusal force. Part 1. measurement and distribution. Am J Orthod Dentofacial Orthop. 1989; 96:493–500. DOI: 10.1016/0889-5406(89)90116-9.39. Strange HE. A three-dimensional consideration of occlusion. Am J Orthod Oral Surg. 1940; 26:787–92. DOI: 10.1016/S0096-6347(40)90333-7.40. Begg PR. Begg orthodontic theory and technique. 1965. Philadelphia: W.B. Saunders Co;p. 60.41. Behrend DA. The mandibular posterior fixed partial denture. J Prosthet Dent. 1977; 37:622–38. DOI: 10.1016/0022-3913(77)90212-8.42. Hood JA, Farah JW, Craig RG. Modification of stresses in alveolar bone induced by a tilted molar. J Prosthet Dent. 1975; 34:415–21. DOI: 10.1016/0022-3913(75)90159-6.43. Sawicka M, Racka-Pilszak B, Rosnowska-Mazurkiewicz A. Uprighting partially impacted permanent second molars. Angle Orthod. 2007; 77:148–154. DOI: 10.2319/010206-461R.1. PMID: 17029525.44. Kraal JH, Digiancinto JJ, Dail RA, Lemmerman K, Peden JW. Periodontal conditions in patients after molar uprighting. J Prosthet Dent. 1980; 43:156–62. DOI: 10.1016/0022-3913(80)90179-1.45. Shiau YY, Peng CC, Hsu CW. Evaluation of biting performance with standardized test foods. J Oral Rehabil. 1999; 26:447–52. DOI: 10.1046/j.1365-2842.1999.00411.x. PMID: 10373094.46. Kohyama K, Hatakeyama E, Sasaki T, Dan H, Azuma T, Karita K. Effects of sample hardness on human chewing force: a model study using silicone rubber. Arch Oral Biol. 2004; 49:805–16. DOI: 10.1016/j.archoralbio.2004.04.006. PMID: 15308425.47. Proffit WR, Fields HW, Nixon WL. Occlusal forces in normal- and long-faced adults. J Dent Res. 1983; 62:566–70. DOI: 10.1177/00220345830620051201. PMID: 6573373.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orthodontic treatment of molar teeth impacted by local factors
- A study on the occlusal wear patterns in maxillary posterior teeth with palatal side abfractions
- An analytical study on strain distribution using strain gauge attached on root surface
- Comparisons of occlusal force according to occlusal relationship, skeletal pattern, age and gender in Koreans
- Occlusal force evaluation and its clinical implication in dental clinics