J Cerebrovasc Endovasc Neurosurg.
2016 Mar;18(1):19-26. 10.7461/jcen.2016.18.1.19.
Delayed Ischemic Stroke after Flow Diversion of Large Posterior Communicating Artery Aneurysm
- Affiliations
-
- 1Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University, Seoul, Korea.
- 2Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University, Seoul, Korea. mh.rho@samsung.com
- KMID: 2161698
- DOI: http://doi.org/10.7461/jcen.2016.18.1.19
Abstract
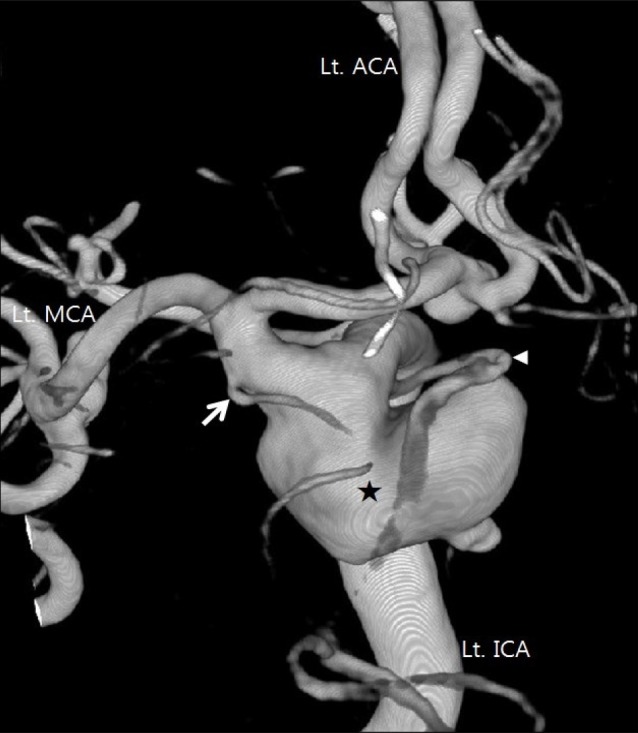
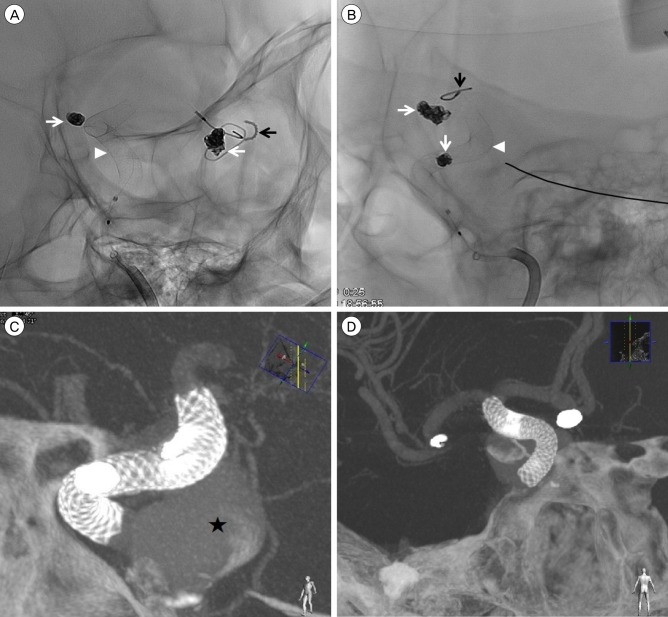
- For securing large, giant, and wide-neck aneurysms, conventional coil embolization has substantial limitations, such as incomplete occlusion, recanalization, and a high recurrence rate. To overcome these limitations, a novel paradigm was suggested and, as a result, flow-diverting device was developed. The flow-diverting device is an innovative and effective technique to allow securing of large, giant, and wide-neck aneurysms. In numerous studies, the flow-diverting device has shown better outcomes than coil embolization. However, the flow-diverting device has also some risks, including rupture of aneurysm, intracerebral hemorrhage, and ischemic stroke. In addition, with more experience, unexpected complications are also reported.5) 7) In the present case, we experienced a delayed ischemic stroke at 27 days after endovascular treatment. The patient had multiple aneurysms and, among them, we treated a large posterior communicating artery aneurysm using Pipelineâ„¢ Embolization Device. The patient was tolerable for 25 days, but then suddenly presented intermittent right hemiparesis. In the initial diffusion magnetic resonance imaging (MRI), there was no acute lesion; however, in the follow-up MRI, an acute ischemic stroke was found in the territory of anterior choroidal artery which was covered by Pipeline Embolization Device. We suspect that neo-intimal overgrowth or a tiny thrombus have led to this delayed complication. Through our case, we learned that the neurosurgeon should be aware of the possibility of delayed ischemic stroke after flow diversion, as well as, long-term close observation and follow-up angiography are necessary even in the event of no acute complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke. 2013; 2. 44(2):442–447. PMID: 23321438.
Article2. Chalouhi N, Tjoumakaris S, Starke RM, Gonzalez LF, Randazzo C, Hasan D, et al. Comparison of flow diversion and coiling in large unruptured intracranial saccular aneurysms. Stroke. 2013; 8. 44(8):2150–2154. PMID: 23723311.
Article3. Chitale R, Gonzalez LF, Randazzo C, Dumont AS, Tjoumakaris S, Rosenwasser R, et al. Single center experience with pipeline stent: feasibility, technique, and complications. Neurosurgery. 2012; 9. 71(3):679–691. PMID: 22653389.4. Chiu AH, Cheung AK, Wenderoth JD, De Villiers L, Rice H, Phatouros CC, et al. Long-term follow-up results following elective treatment of unruptured intracranial aneurysms with the Pipeline embolization device. AJNR Am J Neuroradiol. 2015; 9. 36(9):1728–1734. PMID: 25999412.
Article5. Ding D, Starke RM, Liu KC. Microsurgical strategies following failed endovascular treatment with the pipeline embolization device: case of a giant posterior cerebral artery aneurysm. J Cerebrovasc Endovasc Neurosurg. 2014; 3. 16(1):26–31. PMID: 24765610.
Article6. Eller JL, Dumont TM, Sorkin GC, Mokin M, Levy EI, Snyder KV, et al. The Pipeline embolization device for treatment of intracranial aneurysms. Expert Rev Med Devices. 2014; 3. 11(2):137–150. PMID: 24506298.
Article7. Fiorella D, Hsu D, Woo HH, Tarr RW, Nelson PK. Very late thrombosis of a pipeline embolization device construct: case report. Neurosurgery. 2010; 9. 67(3 Suppl Operative):onsE313–onsE314. discussion onsE314PMID: 20679914.8. Iosif C, Camilleri Y, Saleme S, Caire F, Yardin C, Ponomarjova S, et al. Diffusion-weighted imaging-detected ischemic lesions associated with flow-diverting stents in intracranial aneurysms: safety, potential mechanisms, clinical outcome, and concerns. J Neurosurg. 2015; 3. 122(3):627–636. PMID: 25559933.
Article9. Jeon HJ, Kim DJ, Kim BM, Lee JW. Pipeline embolization device for giant internal carotid artery aneurysms: 9-month follow-up results of two cases. J Cerebrovasc Endovasc Neurosurg. 2014; 6. 16(2):112–118. PMID: 25045651.
Article10. Kallmes DF, Ding YH, Dai D, Kadirvel R, Lewis DA, Cloft HJ. A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke. 2007; 8. 38(8):2346–2352. PMID: 17615366.
Article11. Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonafé A, Cekirge S, et al. International retrospective study of the pipeline embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol. 2015; 1. 36(1):108–115. PMID: 25355814.
Article12. Lall RR, Crobeddu E, Lanzino G, Cloft HJ, Kallmes DF. Acute branch occlusion after Pipeline embolization of intracranial aneurysms. J Clin Neurosci. 2014; 4. 21(4):668–672. PMID: 24156905.
Article13. McDonald RJ, McDonald JS, Kallmes DF, Lanzino G, Cloft HJ. Periprocedural safety of Pipeline therapy for unruptured cerebral aneurysms: Analysis of 279 Patients in a multihospital database. Interv Neuroradiol. 2015; 2. 21(1):6–10. PMID: 25934768.
Article14. Monteith SJ, Tsimpas A, Dumont AS, Tjoumakaris S, Gonzalez LF, Rosenwasser RH, et al. Endovascular treatment of fusiform cerebral aneurysms with the Pipeline Embolization Device. J Neurosurg. 2014; 4. 120(4):945–954. PMID: 24460489.
Article15. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 1. 32(1):34–40. PMID: 21148256.
Article16. Nossek E, Chalif DJ, Chakraborty S, Lombardo K, Black KS, Setton A. Concurrent use of the Pipeline Embolization Device and coils for intracranial aneurysms: technique, safety, and efficacy. J Neurosurg. 2015; 4. 122(4):904–911. PMID: 25658781.
Article17. O'Kelly CJ, Spears J, Chow M, Wong J, Boulton M, Weill A, et al. Canadian experience with the pipeline embolization device for repair of unruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2013; 2. 34(2):381–387. PMID: 22859284.18. Piano M, Valvassori L, Quilici L, Pero G, Boccardi E. Midterm and long-term follow-up of cerebral aneurysms treated with flow diverter devices: a single-center experience. J Neurosurg. 2013; 2. 118(2):408–416. PMID: 23176329.
Article19. Saatci I, Yavuz K, Ozer C, Geyik S, Cekirge HS. Treatment of intracranial aneurysms using the pipeline flow-diverter embolization device: a single-center experience with long-term follow-up results. AJNR Am J Neuroradiol. 2012; 9. 33(8):1436–1446. PMID: 22821921.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis of the Pattern of Anterior-Posterior Circulation in Patients with Posterior Communicating Artery Aneurysm
- True Posterior Communicating Artery Aneurysm
- Physiologic Flow Diversion Coiling Technique for Wide-Necked Aneurysms with an Asymmetric Bidirectional Flow at the Aneurysm Neck
- Transposition of Anterior Choroidal Artery and Posterior Communicating Artery Origin
- Two cases of acute ischemic stroke associated with strut exposure in the cerebral artery lumen after stent-assisted coil embolization