Investig Magn Reson Imaging.
2016 Mar;20(1):1-8. 10.13104/imri.2016.20.1.1.
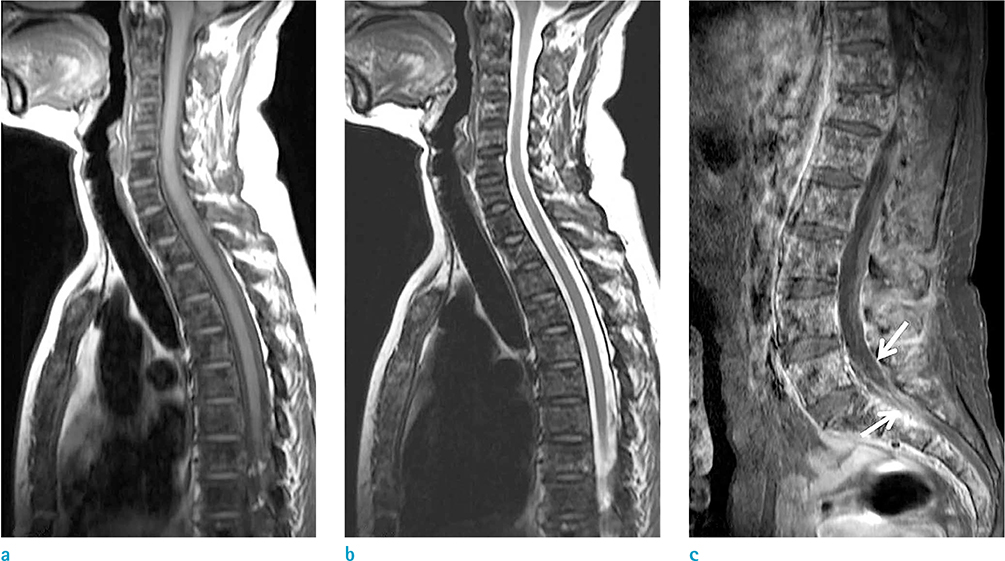
Interpretation of MR Imaging of Spinal Metastasis: Focus on the Understanding of Its Pathophysiology and the Next Step toward a Further Clinical Approach Using MRI Findings
- Affiliations
-
- 1Department of Radiology, Jeju National University Hospital, Jeju, Korea. we1977@naver.com
- KMID: 2161365
- DOI: http://doi.org/10.13104/imri.2016.20.1.1
Abstract
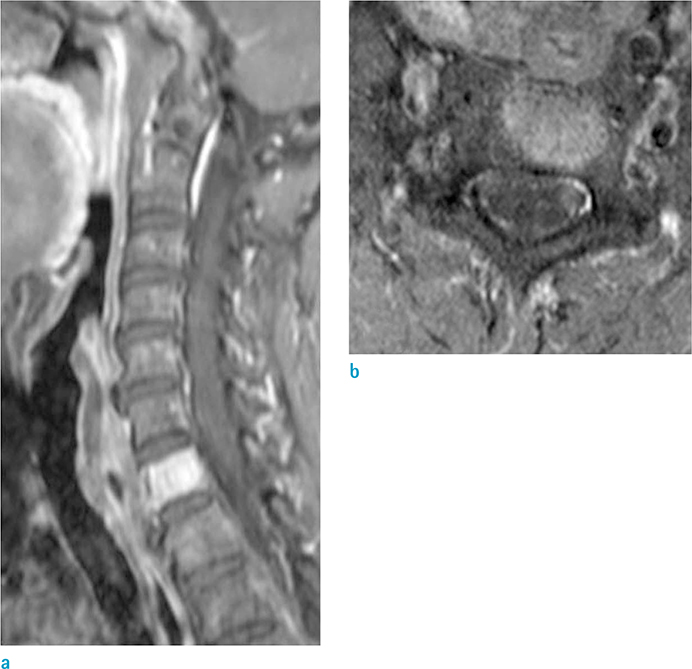
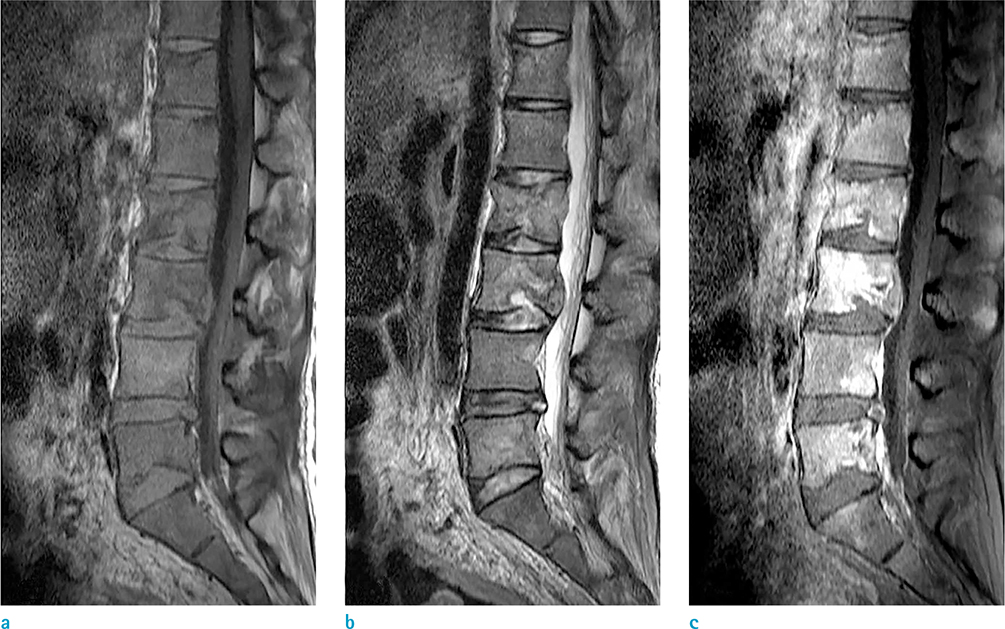
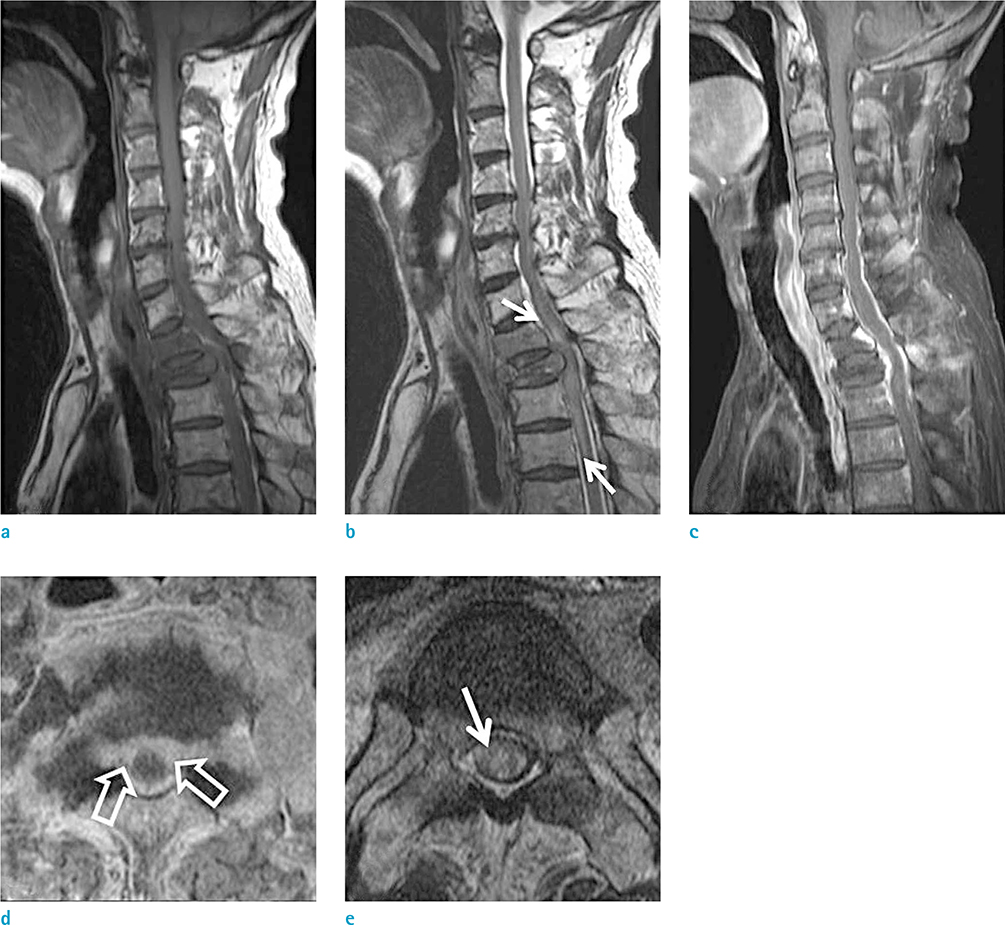
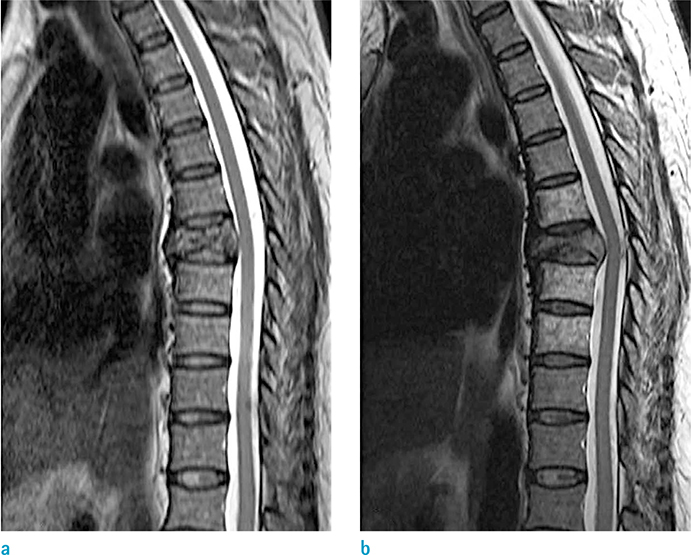
- The spine is the most common location for skeletal metastases, and the incidence of spinal metastasis shows an increasing tendency. Because metastatic spinal tumors progress from an anterior element to a posterior element resulting in continuing destruction of the pedicles, epidural extension and involvement of neural structures of the metastatic tumor are eventually visible. Therefore, it is clinically significant for radiologists to understand the pathophysiology of spinal metastasis and to assess the involvement of neural structures and the disintegration of spinal instability related to the pathophysiology. As MRI is also the best imaging modality for diagnosing spinal metastasis, radiologists should accurately assess spinal metastasis and provide practical information to physicians. Therefore, we will describe some analysis points focusing on the understanding of pathophysiology of spinal metastasis and the next step toward a more extensive clinical approach using MR imaging.
Keyword
Figure
Reference
-
1. Choi D, Crockard A, Bunger C, et al. Review of metastatic spine tumour classification and indications for surgery: the consensus statement of the Global Spine Tumour Study Group. Eur Spine J. 2010; 19:215–222.2. Harel R, Angelov L. Spine metastases: current treatments and future directions. Eur J Cancer. 2010; 46:2696–2707.3. Sciubba DM, Gokaslan ZL. Diagnosis and management of metastatic spine disease. Surg Oncol. 2006; 15:141–151.4. Ecker RD, Endo T, Wetjen NM, Krauss WE. Diagnosis and treatment of vertebral column metastases. Mayo Clin Proc. 2005; 80:1177–1186.5. Mut M, Schiff D, Shaffrey ME. Metastasis to nervous system: spinal epidural and intramedullary metastases. J Neurooncol. 2005; 75:43–56.6. Cole JS, Patchell RA. Metastatic epidural spinal cord compression. Lancet Neurol. 2008; 7:459–466.7. Dunning EC, Butler JS, Morris S. Complications in the management of metastatic spinal disease. World J Orthop. 2012; 3:114–121.8. Schick U, Marquardt G, Lorenz R. Intradural and extradural spinal metastases. Neurosurg Rev. 2001; 24:1–5. discussion 6-79. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001; 26:298–306.10. Galasko CS, Norris HE, Crank S. Spinal instability secondary to metastatic cancer. J Bone Joint Surg Am. 2000; 82:570–594.11. Helweg-Larsen S, Sorensen PS. Symptoms and signs in metastatic spinal cord compression: a study of progression from first symptom until diagnosis in 153 patients. Eur J Cancer. 1994; 30A:396–398.12. Fisher CG, DiPaola CP, Ryken TC, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010; 35:E1221–E1229.13. Crim JR, Bassett LW, Gold RH, et al. Spinal neuroarthropathy after traumatic paraplegia. AJNR Am J Neuroradiol. 1988; 9:359–362.14. Laufer I, Rubin DG, Lis E, et al. The NOMS framework: approach to the treatment of spinal metastatic tumors. Oncologist. 2013; 18:744–751.15. Lee CS, Jung CH. Metastatic spinal tumor. Asian Spine J. 2012; 6:71–87.16. Fisher CG, Versteeg AL, Schouten R, et al. Reliability of the spinal instability neoplastic scale among radiologists: an assessment of instability secondary to spinal metastases. AJR Am J Roentgenol. 2014; 203:869–874.17. Chamberlain MC. Neoplastic meningitis. Neurologist. 2006; 12:179–187.18. Shapiro WR, Johanson CE, Boogerd W. Treatment modalities for leptomeningeal metastases. Semin Oncol. 2009; 36:S46–S54.19. Mostardi PM, Diehn FE, Rykken JB, et al. Intramedullary spinal cord metastases: visibility on PET and correlation with MRI features. AJNR Am J Neuroradiol. 2014; 35:196–201.20. Lee SS, Kim MK, Sym SJ, et al. Intramedullary spinal cord metastases: a single-institution experience. J Neurooncol. 2007; 84:85–89.21. Eastley N, Newey M, Ashford RU. Skeletal metastases - the role of the orthopaedic and spinal surgeon. Surg Oncol. 2012; 21:216–222.22. Love RR, Leventhal H, Easterling DV, Nerenz DR. Side effects and emotional distress during cancer chemotherapy. Cancer. 1989; 63:604–612.23. Cho JH, Ha JK, Hwang CJ, Lee DH, Lee CS. Patterns of treatment for metastatic pathological fractures of the spine: the efficacy of each treatment modality. Clin Orthop Surg. 2015; 7:476–482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging Grading Systems for Central Canal and Neural Foraminal Stenoses of the Lumbar and Cervical Spines With a Focus on the Lee Grading System
- An Updated Review of Magnetic Resonance Neurography for Plexus Imaging
- Understanding the Pathophysiology and Magnetic Resonance Imaging of Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorders
- Magnetic Resonance Imaging of Placenta Accreta Spectrum: A Step-by-Step Approach
- Spinal Presentation of Spontaneous Intracranial Hypotension