J Gynecol Oncol.
2015 Jul;26(3):222-226. 10.3802/jgo.2015.26.3.222.
Robotic high para-aortic lymph node dissection with high port placement using same port for pelvic surgery in gynecologic cancer patients
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tj28.kim@gmail.com
- 2Department of Obstetrics and Gynecology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2160809
- DOI: http://doi.org/10.3802/jgo.2015.26.3.222
Abstract
OBJECTIVE
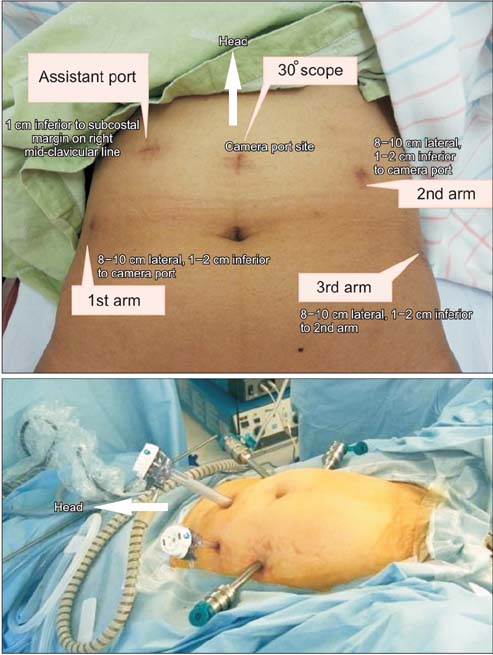
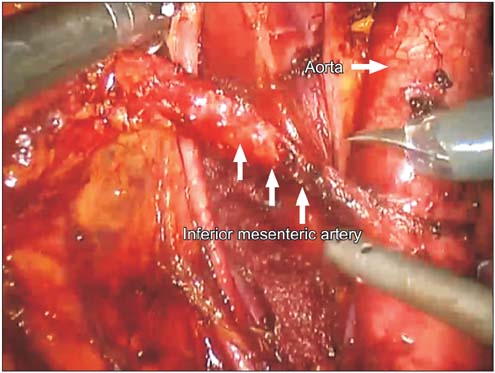
This study reports our initial experience of robotic high para-aortic lymph node dissection (PALND) with high port placement using same port for pelvic surgery in cervical and endometrial cancer patients.
METHODS
Between July 2013 and January 2014, we performed robotic high PALND up to the left renal vein during staging surgeries. With high port placement and same port usage for pelvic surgery, high PALND was successfully performed without repositioning the robotic column. All data were registered consecutively and analyzed retrospectively.
RESULTS
All patients successfully underwent robotic high PALND, followed by hysterectomy and pelvic lymph node dissection. Median age was 45 years (range, 39 to 51 years) and median body mass index was 22 kg/m2 (range, 19.3 to 23.1 kg/m2). Median operative time for right PALND and left PALND was 37 minutes (range, 22 to 65 minutes) and 44 minutes (range, 36 to 50 minutes), respectively. Median number of right and left para-aortic lymph node by pathologic report was 12 (range, 8 to 15) and 13 (range, 5 to 26).
CONCLUSION
With high port placement and one assistant port, robotic high PALND with the same port used in pelvic surgery is feasible to non-obese patients.
Keyword
MeSH Terms
-
Adult
Endometrial Neoplasms/*surgery
Feasibility Studies
Female
Humans
Intraoperative Complications/etiology
Laparoscopy/instrumentation/*methods
Lymph Node Excision/instrumentation/*methods
Lymphatic Metastasis
Middle Aged
Operative Time
Retrospective Studies
Robotic Surgical Procedures/instrumentation/*methods
Surgical Instruments
Uterine Cervical Neoplasms/*surgery
Figure
Cited by 1 articles
-
Robotic lower pelvic port placement for optimal upper paraaortic lymph node dissection
Jiheum Paek, Elizabeth Kang, Peter C. Lim
J Gynecol Oncol. 2018;29(6):. doi: 10.3802/jgo.2018.29.e87.
Reference
-
1. Possover M, Krause N, Plaul K, Kuhne-Heid R, Schneider A. Laparoscopic para-aortic and pelvic lymphadenectomy: experience with 150 patients and review of the literature. Gynecol Oncol. 1998; 71:19–28.2. Kjorstad KE, Kolbenstvedt A, Strickert T. The value of complete lymphadenectomy in radical treatment of cancer of the cervix, stage IB. Cancer. 1984; 54:2215–2219.3. Magrina JF, Long JB, Kho RM, Giles DL, Montero RP, Magtibay PM. Robotic transperitoneal infrarenal aortic lymphadenectomy: technique and results. Int J Gynecol Cancer. 2010; 20:184–187.4. Magrina JF, Kho R, Montero RP, Magtibay PM, Pawlina W. Robotic extraperitoneal aortic lymphadenectomy: development of a technique. Gynecol Oncol. 2009; 113:32–35.5. Jacob KA, Zanagnolo V, Magrina JF, Magtibay PM. Robotic transperitoneal infrarenal aortic lymphadenectomy for gynecologic malignancy: a left lateral approach. J Laparoendosc Adv Surg Tech A. 2011; 21:733–736.6. Holloway RW, Ahmad S. Robotic-assisted surgery in the management of endometrial cancer. J Obstet Gynaecol Res. 2012; 38:1–8.7. Mariani A, Webb MJ, Keeney GL, Podratz KC. Routes of lymphatic spread: a study of 112 consecutive patients with endometrial cancer. Gynecol Oncol. 2001; 81:100–104.8. Mariani A, Dowdy SC, Cliby WA, Gostout BS, Jones MB, Wilson TO, et al. Prospective assessment of lymphatic dissemination in endometrial cancer: a paradigm shift in surgical staging. Gynecol Oncol. 2008; 109:11–18.9. Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009; 27:5331–5336.10. Lee EJ, Kim TJ, Choi CH, Lee JW, Lee JH, Bae DS, et al. Uterine endometrial carcinoma: 10 years' experience with long-term follow-up at a single Korean institution. Gynecol Obstet Invest. 2012; 74:313–319.11. Fastrez M, Vandromme J, George P, Rozenberg S, Degueldre M. Robot assisted laparoscopic transperitoneal para-aortic lymphadenectomy in the management of advanced cervical carcinoma. Eur J Obstet Gynecol Reprod Biol. 2009; 147:226–229.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic lower pelvic port placement for optimal upper paraaortic lymph node dissection
- Single-port laparoscopic transperitoneal infrarenal para-aortic lymphadenectomy as part of staging operation for early ovarian cancer and high grade endometrial cancer
- Laparoscopic Para-aortic Lymph Node Dissection in Patients with Gynecologic Malignancy
- Single-port plus an additional port robotic complete mesocolic excision and intracorporeal anastomosis using a robotic stapler for right-sided colon cancer
- Surgical technique of two-step pelvic and para-aortic sentinel lymph node mapping in early-stage endometrial cancer: laparoscopic, robotic, and open method