Korean J Radiol.
2015 Oct;16(5):1104-1108. 10.3348/kjr.2015.16.5.1104.
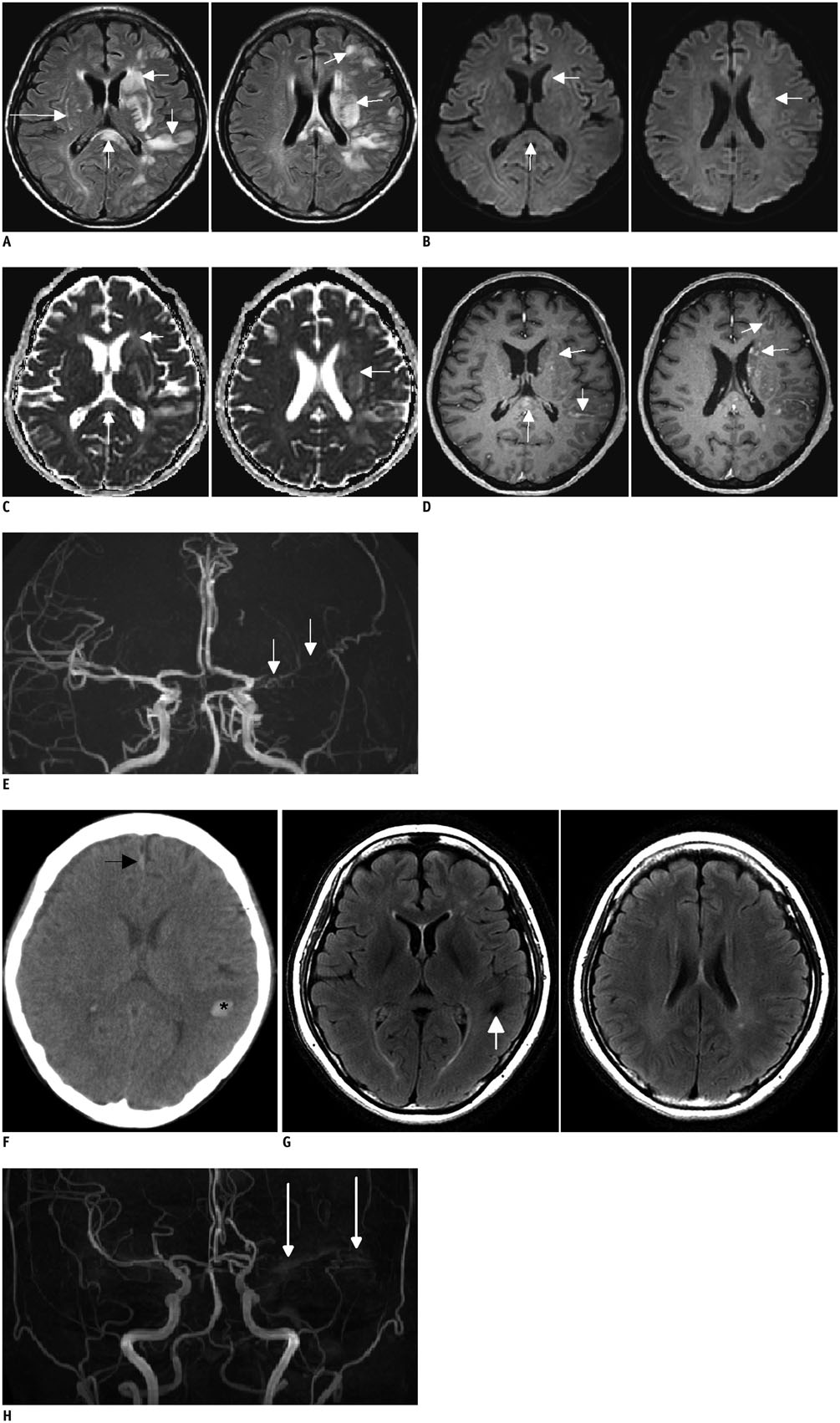
Atypical Unilateral Posterior Reversible Encephalopathy Syndrome Mimicking a Middle Cerebral Artery Infarction
- Affiliations
-
- 1Department of Radiology, Ondokuz Mayis University, Faculty of Medicine, Kurupelit 55220, Samsun, Turkey. ilkayozaydin@hotmail.com
- 2Department of Neurology, Yonsei University Severance Hospital, Seoul 03722, Korea.
- 3Department of Radiology, Yonsei University Severance Hospital, Seoul 03722, Korea.
- KMID: 2160778
- DOI: http://doi.org/10.3348/kjr.2015.16.5.1104
Abstract
- Posterior reversible encephalopathy syndrome (PRES) is usually a reversible clinical and radiological entity associated with typical features on brain MR or CT imaging. However, the not-so-uncommon atypical radiological presentations of the condition are also present and they may go unrecognised as they are confused with other conditions. Here, we report a very rare case of atypical, unilateral PRES in a 49-year-old uremic, post-transplant female patient who presented with seizures. Initial MRI showed high-grade occlusion of the left middle cerebral artery (MCA) and lesions suggestive of subacute infarction in the ipsilateral frontotemporoparietal lobe. Patient symptoms had resolved a day after the onset without any specific treatment but early follow-up CT findings suggested hemorrhagic transformation. Follow-up MRI performed 2 years later showed complete disappearence of the lesions and persisting MCA occlusion.
MeSH Terms
Figure
Reference
-
1. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996; 334:494–500.2. Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. AJNR Am J Neuroradiol. 2008; 29:1036–1042.3. McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, et al. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol. 2007; 189:904–912.4. McKinney AM, Jagadeesan BD, Truwit CL. Central-variant posterior reversible encephalopathy syndrome: brainstem or basal ganglia involvement lacking cortical or subcortical cerebral edema. AJR Am J Roentgenol. 2013; 201:631–638.5. Hugonnet E, Da Ines D, Boby H, Claise B, Petitcolin V, Lannareix V, et al. Posterior reversible encephalopathy syndrome (PRES): features on CT and MR imaging. Diagn Interv Imaging. 2013; 94:45–52.6. Schambra HM, Greer DM. Asymmetric reversible posterior leukoencephalopathy syndrome. Neurocrit Care. 2006; 4:245–247.7. Covarrubias DJ, Luetmer PH, Campeau NG. Posterior reversible encephalopathy syndrome: prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol. 2002; 23:1038–1048.8. Hefzy HM, Bartynski WS, Boardman JF, Lacomis D. Hemorrhage in posterior reversible encephalopathy syndrome: imaging and clinical features. AJNR Am J Neuroradiol. 2009; 30:1371–1379.9. McKinney AM, Sarikaya B, Gustafson C, Truwit CL. Detection of microhemorrhage in posterior reversible encephalopathy syndrome using susceptibility-weighted imaging. AJNR Am J Neuroradiol. 2012; 33:896–903.10. Dhar R, Dacey R, Human T, Zipfel G. Unilateral posterior reversible encephalopathy syndrome with hypertensive therapy of contralateral vasospasm: case report. Neurosurgery. 2011; 69:E1176–E1181. E118111. Voetsch B, Tarlov N, Nguyen TN, DeFusco C, Barest GD, Norbash A, et al. Asymmetric posterior reversible encephalopathy syndrome complicating hemodynamic augmentation for subarachnoid hemorrhage-associated cerebral vasospasm. Neurocrit Care. 2011; 15:542–546.12. Romano A, Silvia P, Alberto P, Tavanti F, Sette G, La Starza S, et al. Asymmetric posterior reversible encephalopathy syndrome in patient with hyperplastic anterior choroidal artery. J Headache Pain. 2011; 12:259–261.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Reversible Encephalopathy Syndrome with Extensive Brain Involvement Accompanied by Cerebral Infarction
- Reversible Cerebral Vasoconstriction Syndrome Combined with Posterior Encephalopathy Syndrome, and Transient Splenial Lesion after Delivery
- Bilateral Anterior Cerebral Artery Infarction Associated with Reversible Cerebral Vasoconstriction Syndrome
- Posterior Reversible Encephalopathy Syndrome in a Patient with Intoxication of Arisaema amurense
- Hypertensive Brainstem Encephalopathy Combined with Acute Ischemic Stroke