Obstet Gynecol Sci.
2016 Mar;59(2):97-102. 10.5468/ogs.2016.59.2.97.
Preoperative and postoperative serum C-reactive protein levels to predict the outcome of ultrasound-indicated cerclage
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kangnam Sacred Heart Hospital, Hallym University Medical Center, Hallym University College of Medicine, Seoul, Korea. guittool@hallym.or.kr
- KMID: 2159003
- DOI: http://doi.org/10.5468/ogs.2016.59.2.97
Abstract
OBJECTIVE
To assess the role of preoperative and postoperative serum C-reactive protein (CRP) level on the prediction of pregnancy outcomes following ultrasound-indicated cerclage (UIC).
METHODS
We retrospectively reviewed the medical records 44 women who underwent UIC between January 2011 and December 2011. UIC was performed between 14 and 24 weeks of gestation in women with short cervix. We divided UIC patients into two groups according to the gestational age at delivery (34 weeks) and compared the two groups. Group A was defined as patients who delivered ≥34 weeks of gestation, and group B as patients delivered <34 weeks. Correlation and receiver-operating characteristic curves were also analyzed for the prediction of preterm birth after UIC.
RESULTS
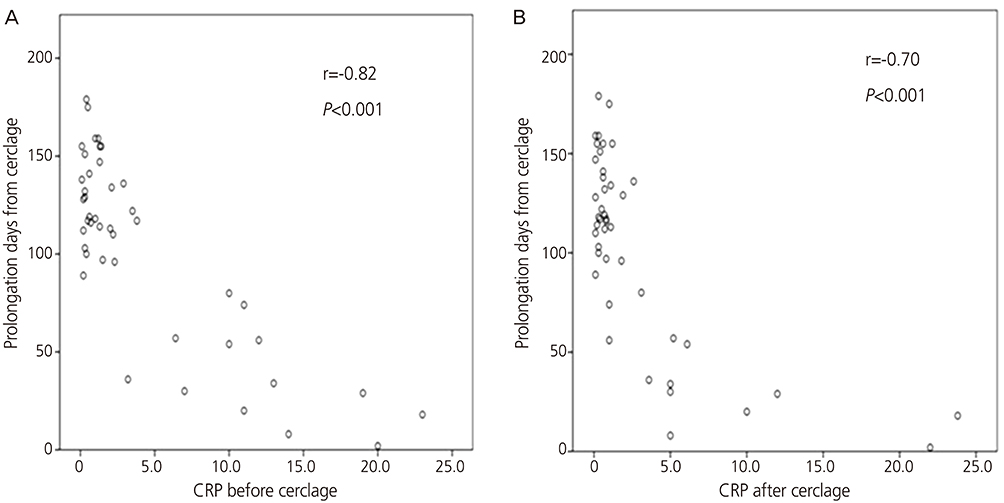
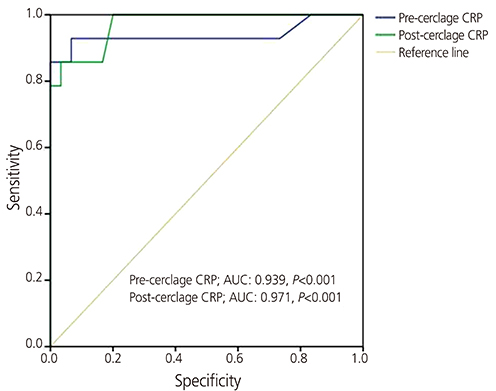
Thirty women delivered ≥34 weeks (group A) and 14 women delivered <34 weeks (group B). Pre- and post-cerclage CRP were significantly lower in group A (pre-cerclage CRP, 1.1±1.0 vs. 11.4±6.2 mg/dL, P<0.001; post-cerclage CRP, 0.6±0.5 vs. 7.4±7.2 mg/dL, P<0.001). The mean gestational age at delivery in group A was 37.7±1.8 weeks and that in group B was 26.9±4.3 weeks (P<0.001). There were significant negative correlations between pre- and post-cerclage CRP and latency from UIC to delivery (r=-0.82, P<0.001; r=-0.70, P<0.001, respectively).
CONCLUSION
Both pre- and post-cerclage CRP were useful in predicting the preterm birth following UIC.
MeSH Terms
Figure
Reference
-
1. Kwak DW, Cho HY, Kwon JY, Park YW, Kim YH. Usefulness of maternal serum C-reactive protein with vaginal Ureaplasma urealyticum as a marker for prediction of imminent preterm delivery and chorioamnionitis in patients with preterm labor or preterm premature rupture of membranes. J Perinat Med. 2015; 43:409–415.2. Ahmed SK, Mahmood N, Malalla ZH, Alsobyani FM, Al-Kiyumi IS, Almawi WY. C-reactive protein gene variants associated with recurrent pregnancy loss independent of CRP serum levels: a case-control study. Gene. 2015; 569:136–140.3. Lohsoonthorn V, Qiu C, Williams MA. Maternal serum C-reactive protein concentrations in early pregnancy and subsequent risk of preterm delivery. Clin Biochem. 2007; 40(5-6):330–335.4. Best LG, Saxena R, Anderson CM, Barnes MR, Hakonarson H, Falcon G, et al. Two variants of the C-reactive protein gene are associated with risk of pre-eclampsia in an American Indian population. PLoS One. 2013; 8:e71231.5. Tjoa ML, van Vugt JM, Go AT, Blankenstein MA, Oudejans CB, van Wijk IJ. Elevated C-reactive protein levels during first trimester of pregnancy are indicative of preeclampsia and intrauterine growth restriction. J Reprod Immunol. 2003; 59:29–37.6. Morales E, Guerra S, Garcia-Esteban R, Guxens M, Alvarez-Pedrerol M, Bustamante M, et al. Maternal C-reactive protein levels in pregnancy are associated with wheezing and lower respiratory tract infections in the offspring. Am J Obstet Gynecol. 2011; 204:164.e1–164.e9.7. Berghella V, Rafael TJ, Szychowski JM, Rust OA, Owen J. Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: a meta-analysis. Obstet Gynecol. 2011; 117:663–671.8. Nelson L, Dola T, Tran T, Carter M, Luu H, Dola C. Pregnancy outcomes following placement of elective, urgent and emergent cerclage. J Matern Fetal Neonatal Med. 2009; 22:269–273.9. Chan LL, Leung TW, Lo TK, Lau WL, Leung WC. Indications for and pregnancy outcomes of cervical cerclage: 11-year comparison of patients undergoing history-indicated, ultrasound-indicated, or rescue cerclage. Hong Kong Med J. 2015; 21:310–317.10. Berghella V, Bega G. Ultrasound evaluation of the cervix. In : Callen PW, editor. Ultrasonography in obstetrics and gynecology. 5th ed. Philadelphia (PA): Saunders/Elsevier;2008. p. 698–720.11. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996; 334:567–572.12. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005; 106:181–189.13. Berghella V. Transvaginal ultrasound assessment of the cervix and prediction of spontaneous preterm birth [Internet]. [place unknown]: cited 2016 Feb 6. Available from: http://www.uptodate.com.14. Skupski DW, Lin SN, Reiss J, Eglinton GS. Extremely short cervix in the second trimester: bed rest or modified Shirodkar cerclage? J Perinat Med. 2014; 42:55–59.15. Sakai M, Shiozaki A, Tabata M, Sasaki Y, Yoneda S, Arai T, et al. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol. 2006; 194:14–19.16. Kobayashi M, Ohkuchi A, Matsubara S, Izumi A, Hirashima C, Suzuki M. C-reactive protein levels at pre-/post-indicated cervical cerclage predict very preterm birth. J Perinat Med. 2011; 39:151–155.17. Minakami H, Matsubara S, Izumi A, Kosuge S, Watanabe T, Iwasaki R, et al. Emergency cervical cerclage: relation between its success, preoperative serum level of C-reactive protein and WBC count, and degree of cervical dilatation. Gynecol Obstet Invest. 1999; 47:157–161.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The significance of C-reactive protein levels in maternal serum with outcome of tocolysis
- Analysis of Factors That Affect the Outcome of Skin Grafts
- The Usefulness in the Value of Some Infectious Parameters to Predict the Success of Emergency Cervical Cerclage Operation
- Emergency cerclage in cervical incompetence
- Significance of Erythrocyte Sedimentation Rate and C-reactive Protein as Predictive Factors for Prognosis in Non-metastatic Renal Cell Carcinoma