Yonsei Med J.
2013 Jul;54(4):973-982. 10.3349/ymj.2013.54.4.973.
Stepwise Treatment Using Corticosteroids Alone and in Combination with Cyclosporine in Korean Patients with Idiopathic Membranous Nephropathy
- Affiliations
-
- 1Department of Internal Medicine, Kangdong Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea.
- 2Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. kswkidney@yuhs.ac
- 3Severance Biomedical Science Institute, Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2158234
- DOI: http://doi.org/10.3349/ymj.2013.54.4.973
Abstract
- PURPOSE
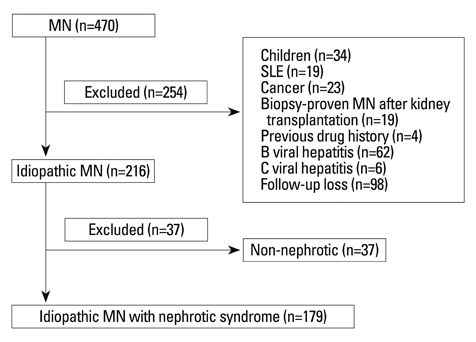
We undertook an observational study to investigate the effects of immunosuppressive treatment on proteinuria and renal function in 179 Korean idiopathic membranous nephropathy patients with nephrotic syndrome.
MATERIALS AND METHODS
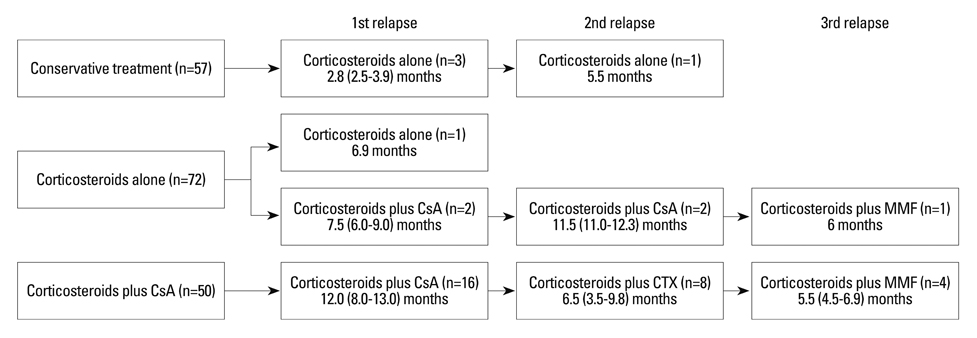
The primary outcome was regarded as the first appearance of remission and the secondary outcomes as a decline in estimated glomerular filtration rate (eGFR) >50% or initiation of dialysis, and all-cause mortality. Seventy-two (40.2%) and 50 (27.9%) patients were treated with corticosteroids alone (C) and corticosteroids plus cyclosporine (C+C), respectively, whereas 57 (31.8%) did not receive immunosuppressants (NTx). Cyclosporine was added if there was no reduction in proteinuria of >50% from baseline by corticosteroids alone within 3 months.
RESULTS
There were no differences in baseline renal function and the amount of proteinuria among the three groups. Overall, complete remission (CR) was achieved in 88 (72.1%) patients by immunosuppressants. In a multivariate analysis adjusted for covariates associated with adverse renal outcome, the probability of reaching CR was significantly higher in the C [hazard ratio (HR), 4.09; p<0.001] and C+C groups (HR, 2.57; p=0.003) than in the NTx group. Kaplan-Meier analysis revealed that 5-year CR rates of C, C+C, and NTx groups were 88.5%, 86.2%, and 56.7% (p<0.001). Ten-year event-free rates for the secondary endpoints in these three groups were 91.7%, 79.9%, and 57.2% (p=0.01).
CONCLUSION
Immunosuppressive treatment was effective in inducing remission and preserving renal function in these patients. Therefore, stepwise treatment using corticosteroids alone and in combination with cyclosporine is warranted in these patients.
Keyword
MeSH Terms
-
Adrenal Cortex Hormones/adverse effects/*therapeutic use
Adult
Aged
Cyclosporine/adverse effects/*therapeutic use
Drug Administration Schedule
Female
Glomerular Filtration Rate/drug effects
Glomerulonephritis, Membranous/*drug therapy/mortality
Humans
Immunosuppressive Agents/adverse effects/*therapeutic use
Kaplan-Meier Estimate
Kidney/drug effects/physiology
Male
Middle Aged
Proteinuria/chemically induced
Treatment Outcome
Adrenal Cortex Hormones
Immunosuppressive Agents
Cyclosporine
Figure
Reference
-
1. Cattran DC. Idiopathic membranous glomerulonephritis. Kidney Int. 2001; 59:1983–1994.
Article2. Ponticelli C, Passerini P. Can prognostic factors assist therapeutic decisions in idiopathic membranous nephropathy? J Nephrol. 2010; 23:156–163.3. Muirhead N. Management of idiopathic membranous nephropathy: evidence-based recommendations. Kidney Int Suppl. 1999; 70:S47–S55.
Article4. Cameron JS, Healy MJ, Adu D. The MRC Glomerulonephritis Working Party. The Medical Research Council trial of short-term high-dose alternate day prednisolone in idiopathic membranous nephropathy with nephrotic syndrome in adults. Q J Med. 1990; 74:133–156.
Article5. Cattran DC, Delmore T, Roscoe J, Cole E, Cardella C, Charron R, et al. A randomized controlled trial of prednisone in patients with idiopathic membranous nephropathy. N Engl J Med. 1989; 320:210–215.
Article6. Glassock RJ. The treatment of idiopathic membranous nephropathy: a dilemma or a conundrum? Am J Kidney Dis. 2004; 44:562–566.
Article7. Ponticelli C, Zucchelli P, Passerini P, Cesana B, Locatelli F, Pasquali S, et al. A 10-year follow-up of a randomized study with methylprednisolone and chlorambucil in membranous nephropathy. Kidney Int. 1995; 48:1600–1604.
Article8. Ponticelli C, Altieri P, Scolari F, Passerini P, Roccatello D, Cesana B, et al. A randomized study comparing methylprednisolone plus chlorambucil versus methylprednisolone plus cyclophosphamide in idiopathic membranous nephropathy. J Am Soc Nephrol. 1998; 9:444–450.
Article9. Ponticelli C, Zucchelli P, Passerini P, Cesana B. The Italian Idiopathic Membranous Nephropathy Treatment Study Group. Methylprednisolone plus chlorambucil as compared with methylprednisolone alone for the treatment of idiopathic membranous nephropathy. N Engl J Med. 1992; 327:599–603.
Article10. Faurschou M, Sorensen IJ, Mellemkjaer L, Loft AG, Thomsen BS, Tvede N, et al. Malignancies in Wegener's granulomatosis: incidence and relation to cyclophosphamide therapy in a cohort of 293 patients. J Rheumatol. 2008; 35:100–105.11. Wetzels JF. Cyclophosphamide-induced gonadal toxicity: a treatment dilemma in patients with lupus nephritis? Neth J Med. 2004; 62:347–352.12. du Buf-Vereijken PW, Branten AJ, Wetzels JF. Membranous Nephropathy Study Group. Cytotoxic therapy for membranous nephropathy and renal insufficiency: improved renal survival but high relapse rate. Nephrol Dial Transplant. 2004; 19:1142–1148.
Article13. Eriguchi M, Oka H, Mizobuchi T, Kamimura T, Sugawara K, Harada A. Long-term outcomes of idiopathic membranous nephropathy in Japanese patients treated with low-dose cyclophosphamide and prednisolone. Nephrol Dial Transplant. 2009; 24:3082–3088.
Article14. Shiiki H, Saito T, Nishitani Y, Mitarai T, Yorioka N, Yoshimura A, et al. Prognosis and risk factors for idiopathic membranous nephropathy with nephrotic syndrome in Japan. Kidney Int. 2004; 65:1400–1407.
Article15. Tang S, Chan TM, Cheng IK, Lai KN. Clinical features and treatment outcome of idiopathic membranous nephropathy in Chinese patients. QJM. 1999; 92:401–406.
Article16. Cattran DC, Appel GB, Hebert LA, Hunsicker LG, Pohl MA, Hoy WE, et al. Cyclosporine in patients with steroid-resistant membranous nephropathy: a randomized trial. Kidney Int. 2001; 59:1484–1490.
Article17. Cattran DC, Greenwood C, Ritchie S, Bernstein K, Churchill DN, Clark WF, et al. Canadian Glomerulonephritis Study Group. A controlled trial of cyclosporine in patients with progressive membranous nephropathy. Kidney Int. 1995; 47:1130–1135.
Article18. Ehrenreich T, Churg J. Pathology of membranous nephropathy. Pathol Annu. 1968; 3:145–186.19. Youn YS, Lim HH, Lee JH. The clinical characteristics of steroid responsive nephrotic syndrome of children according to the serum immunoglobulin E levels and cytokines. Yonsei Med J. 2012; 53:715–722.
Article20. Hofstra JM, Wetzels JF. Alkylating agents in membranous nephropathy: efficacy proven beyond doubt. Nephrol Dial Transplant. 2010; 25:1760–1766.
Article21. du Buf-Vereijken PW, Branten AJ, Wetzels JF. Idiopathic membranous nephropathy: outline and rationale of a treatment strategy. Am J Kidney Dis. 2005; 46:1012–1029.
Article22. Cattran D. Management of membranous nephropathy: when and what for treatment. J Am Soc Nephrol. 2005; 16:1188–1194.
Article23. Cattran DC, Alexopoulos E, Heering P, Hoyer PF, Johnston A, Meyrier A, et al. Cyclosporin in idiopathic glomerular disease associated with the nephrotic syndrome: workshop recommendations. Kidney Int. 2007; 72:1429–1447.
Article24. Alexopoulos E, Papagianni A, Tsamelashvili M, Leontsini M, Memmos D. Induction and long-term treatment with cyclosporine in membranous nephropathy with the nephrotic syndrome. Nephrol Dial Transplant. 2006; 21:3127–3132.
Article25. Polanco N, Gutiérrez E, Covarsí A, Ariza F, Carreño A, Vigil A, et al. Spontaneous remission of nephrotic syndrome in idiopathic membranous nephropathy. J Am Soc Nephrol. 2010; 21:697–704.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of idiopathic membranous nephropathy treated with rituximab
- A case of membranous nephropathy associated with relapsing polychondritis
- Membranous Nephropathy in a 13-Year-Old Boy with Common Variable Immunodeficiency
- The Effect of Mycophenolate Mofetil versus Cyclosporine as Combination Therapy with Low Dose Corticosteroids in High-risk Patients with Idiopathic Membranous Nephropathy: a Multicenter Randomized Trial
- Expression of Glomerular-Smooth Muscle Actin and Vimentin in Idiopathic Membranous Nephropathy as Prognostic Indicators