Yonsei Med J.
2013 Jul;54(4):942-948. 10.3349/ymj.2013.54.4.942.
Associations of Moderate to Severe Asthma with Obstructive Sleep Apnea
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Division of Pulmonology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. pms70@yuhs.ac
- 3The Institute of Chest Diseases, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2158230
- DOI: http://doi.org/10.3349/ymj.2013.54.4.942
Abstract
- PURPOSE
This study aimed to evaluate the correlation between associating factors of moderate to severe asthma with obstructive sleep apnea (OSA).
MATERIALS AND METHODS
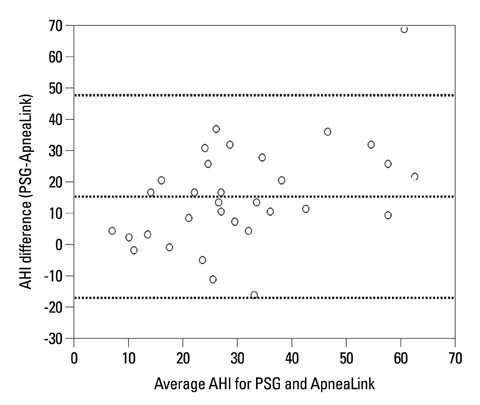
One hundred and sixty-seven patients who visited the pulmonary and sleep clinic in Severance Hospital presenting with symptoms of sleep-disordered breathing were evaluated. All subjects were screened with ApneaLink. Thirty-two subjects with a high likelihood of having OSA were assessed with full polysomnography (PSG).
RESULTS
The mean age was 58.8+/-12.0 years and 58.7% of subjects were male. The mean ApneaLink apnea-hypopnea index (AHI) was 12.7+/-13.0/hr. The mean ApneaLink AHI for the 32 selected high risk patients of OSA was 22.3+/-13.2/hr, which was lower than the sleep laboratory-based PSG AHI of 39.1+/-20.5/hr. When OSA was defined at an ApneaLink AHI > or =5/hr, the positive correlating factors for OSA were age, male gender, and moderate to severe asthma.
CONCLUSION
Moderate to severe asthma showed strong correlation with OSA when defined at an ApneaLink AHI > or =5/hr.
Keyword
MeSH Terms
Figure
Reference
-
1. Tishler PV, Larkin EK, Schluchter MD, Redline S. Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. JAMA. 2003; 289:2230–2237.
Article2. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002; 165:1217–1239.3. Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004; 170:1108–1113.
Article4. Larsson LG, Lindberg A, Franklin KA, Lundbäck B. Symptoms related to obstructive sleep apnoea are common in subjects with asthma, chronic bronchitis and rhinitis in a general population. Respir Med. 2001; 95:423–429.
Article5. Janson C, De Backer W, Gislason T, Plaschke P, Björnsson E, Hetta J, et al. Increased prevalence of sleep disturbances and daytime sleepiness in subjects with bronchial asthma: a population study of young adults in three European countries. Eur Respir J. 1996; 9:2132–2138.
Article6. Fitzpatrick MF, Martin K, Fossey E, Shapiro CM, Elton RA, Douglas NJ. Snoring, asthma and sleep disturbance in Britain: a community-based survey. Eur Respir J. 1993; 6:531–535.7. Knuiman M, James A, Divitini M, Bartholomew H. Longitudinal study of risk factors for habitual snoring in a general adult population: the Busselton Health Study. Chest. 2006; 130:1779–1783.
Article8. Yigla M, Tov N, Solomonov A, Rubin AH, Harlev D. Difficult-to-control asthma and obstructive sleep apnea. J Asthma. 2003; 40:865–871.
Article9. Ciftci TU, Ciftci B, Guven SF, Kokturk O, Turktas H. Effect of nasal continuous positive airway pressure in uncontrolled nocturnal asthmatic patients with obstructive sleep apnea syndrome. Respir Med. 2005; 99:529–534.
Article10. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007; 120:5 Suppl. S94–S138.11. Kasasbeh A, Kasasbeh E, Krishnaswamy G. Potential mechanisms connecting asthma, esophageal reflux, and obesity/sleep apnea complex--a hypothetical review. Sleep Med Rev. 2007; 11:47–58.
Article12. Arter JL, Chi DS, M G, Fitzgerald SM, Guha B, Krishnaswamy G. Obstructive sleep apnea, inflammation, and cardiopulmonary disease. Front Biosci. 2004; 9:2892–2900.
Article13. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999; 22:667–689.14. Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Wheatley J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med. 2004; 169:668–672.15. Whittle AT, Finch SP, Mortimore IL, MacKay TW, Douglas NJ. Use of home sleep studies for diagnosis of the sleep apnoea/hypopnoea syndrome. Thorax. 1997; 52:1068–1073.
Article16. Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, et al. Portable Monitoring Task Force of the American Academy of Sleep Medicine. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. J Clin Sleep Med. 2007; 3:737–747.17. Ng SS, Chan TO, To KW, Ngai J, Tung A, Ko FW, et al. Validation of a portable recording device (ApneaLink) for identifying patients with suspected obstructive sleep apnoea syndrome. Intern Med J. 2009; 39:757–762.
Article18. Erman MK, Stewart D, Einhorn D, Gordon N, Casal E. Validation of the ApneaLink for the screening of sleep apnea: a novel and simple single-channel recording device. J Clin Sleep Med. 2007; 3:387–392.
Article19. Hui DS, To KW, Ko FW, Fok JP, Chan MC, Ngai JC, et al. Nasal CPAP reduces systemic blood pressure in patients with obstructive sleep apnoea and mild sleepiness. Thorax. 2006; 61:1083–1090.
Article20. American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med. 2000; 162:2341–2351.21. Pepe C, Foley S, Shannon J, Lemiere C, Olivenstein R, Ernst P, et al. Differences in airway remodeling between subjects with severe and moderate asthma. J Allergy Clin Immunol. 2005; 116:544–549.
Article22. Hui DS, Ko FW, Fok JP, Chan MC, Li TS, Tomlinson B, et al. The effects of nasal continuous positive airway pressure on platelet activation in obstructive sleep apnea syndrome. Chest. 2004; 125:1768–1775.
Article23. Teodorescu M, Consens FB, Bria WF, Coffey MJ, McMorris MS, Weatherwax KJ, et al. Correlates of daytime sleepiness in patients with asthma. Sleep Med. 2006; 7:607–613.
Article24. Alharbi M, Almutairi A, Alotaibi D, Alotaibi A, Shaikh S, Bahammam AS. The prevalence of asthma in patients with obstructive sleep apnoea. Prim Care Respir J. 2009; 18:328–330.
Article25. Julien JY, Martin JG, Ernst P, Olivenstein R, Hamid Q, Lemière C, et al. Prevalence of obstructive sleep apnea-hypopnea in severe versus moderate asthma. J Allergy Clin Immunol. 2009; 124:371–376.
Article26. Bonekat HW, Hardin KA. Severe upper airway obstruction during sleep. Clin Rev Allergy Immunol. 2003; 25:191–210.
Article27. Bohadana AB, Hannhart B, Teculescu DB. Nocturnal worsening of asthma and sleep-disordered breathing. J Asthma. 2002; 39:85–100.
Article28. Catterall JR, Douglas NJ, Calverley PM, Brash HM, Brezinova V, Shapiro CM, et al. Irregular breathing and hypoxaemia during sleep in chronic stable asthma. Lancet. 1982; 1:301–304.
Article29. Mastronarde JG, Wise RA, Shade DM, Olopade CO, Scharf SM. American Lung Association Asthma Clinical Research Centers. Sleep quality in asthma: results of a large prospective clinical trial. J Asthma. 2008; 45:183–189.
Article30. Johns MW. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest. 1993; 103:30–36.
Article31. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000; 342:1378–1384.
Article32. Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001; 163:19–25.
Article33. Ip MS, Lam B, Lauder IJ, Tsang KW, Chung KF, Mok YW, et al. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest. 2001; 119:62–69.
Article34. Li KK, Kushida C, Powell NB, Riley RW, Guilleminault C. Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope. 2000; 110(10 Pt 1):1689–1693.
Article35. Sakakibara H, Tong M, Matsushita K, Hirata M, Konishi Y, Suetsugu S. Cephalometric abnormalities in non-obese and obese patients with obstructive sleep apnoea. Eur Respir J. 1999; 13:403–410.
Article36. Ong KC, Clerk AA. Comparison of the severity of sleep-disordered breathing in Asian and Caucasian patients seen at a sleep disorders center. Respir Med. 1998; 92:843–848.
Article37. Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P, Darendeliler MA, et al. Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep. 2010; 33:1075–1080.
Article38. Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999; 14:902–907.
Article39. Juniper EF, Bousquet J, Abetz L, Bateman ED. GOAL Committee. Identifying 'well-controlled' and 'not well-controlled' asthma using the Asthma Control Questionnaire. Respir Med. 2006; 100:616–621.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric sleep questionnaires for screening of obstructive sleep apnea syndrome
- Allergic Rhinitis and Sleep-disordered Breathing
- A Case of REM-Dependent Obstructive Sleep Apnea Syndrome
- A Case of Huge Lingual Tonsillar Hypertrophy Causing Obstructive Sleep Apnea in Adult
- A 23-year-old female with Down syndrome accompanied by obstructive sleep apnea and acute respiratory failure