J Korean Med Sci.
2012 Nov;27(11):1418-1423. 10.3346/jkms.2012.27.11.1418.
The Incidence, Causes, and Prognostic Significance of New-Onset Thrombocytopenia in Intensive Care Units: A Prospective Cohort Study in a Korean Hospital
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. suhgy@skku.edu
- 2Department of Laboratory Medicine & Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2157956
- DOI: http://doi.org/10.3346/jkms.2012.27.11.1418
Abstract
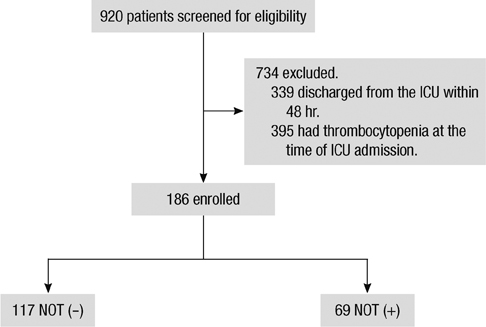
- This study was designed to investigate the incidence, causes, and outcomes of new-onset thrombocytopenia (NOT) in Korean intensive care units (ICUs). A prospective cohort study was conducted in medical ICUs of Samsung Medical Center between August 2010 and February 2011. All newly admitted patients were included if they stayed in the ICU for more than 48 hr and did not have thrombocytopenia upon admission. A total of 186 patients were included. NOT developed in 37.1%. Most common cause of NOT was sepsis with disseminated intravascular coagulation (66.7%), followed by drug-induced thrombocytopenia (18.8%), and heparin-induced thrombocytopenia (2.9%). IgG-specific antibody to platelet factor 4/heparin was positive in 2.4% among patients treated with heparin, and thrombosis occurred in two patients. Twenty eight-day mortality was higher in patients that developed NOT compared to those that did not develop NOT (39.1% vs 12%, P < 0.001). NOT increased the odds ratio of 28-day mortality and was an independent risk factor for mortality (OR 3.52; 95% CI 1.32-9.38; P = 0.012). In conclusion, NOT is common and is an independent risk factor for mortality in Korean ICU patients. Therefore, clinicians should make every effort to correct the causes of NOT.
Keyword
MeSH Terms
-
Aged
Cohort Studies
Disseminated Intravascular Coagulation/complications
Female
Heparin/immunology
Hospitals
Humans
Immunoglobulin G/blood
Incidence
Intensive Care Units
Male
Middle Aged
Odds Ratio
Platelet Factor 4/immunology
Prognosis
Prospective Studies
Republic of Korea
Risk Factors
Sepsis/complications
Survival Analysis
Thrombocytopenia/*epidemiology/etiology/mortality
Thrombosis/etiology
Immunoglobulin G
Platelet Factor 4
Heparin
Figure
Reference
-
1. Bonfiglio MF, Traeger SM, Kier KL, Martin BR, Hulisz DT, Verbeck SR. Thrombocytopenia in intensive care patients: a comprehensive analysis of risk factors in 314 patients. Ann Pharmacother. 1995. 29:835–842.2. Crowther MA, Cook DJ, Meade MO, Griffith LE, Guyatt GH, Arnold DM, Rabbat CG, Geerts WH, Warkentin TE. Thrombocytopenia in medicalsurgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005. 20:348–353.3. Strauss R, Wehler M, Mehler K, Kreutzer D, Koebnick C, Hahn EG. Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Crit Care Med. 2002. 30:1765–1771.4. Lee KH, Hui KP, Tan WC. Thrombocytopenia in sepsis: a predictor of mortality in the intensive care unit. Singapore Med J. 1993. 34:245–246.5. Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM. The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest. 2011. 139:271–278.6. Vanderschueren S, De Weerdt A, Malbrain M, Vankersschaever D, Frans E, Wilmer A, Bobbaers H. Thrombocytopenia and prognosis in intensive care. Crit Care Med. 2000. 28:1871–1876.7. Akca S, Haji-Michael P, de Mendonca A, Suter P, Levi M, Vincent JL. Time course of platelet counts in critically ill patients. Crit Care Med. 2002. 30:753–756.8. Shalansky SJ, Verma AK, Levine M, Spinelli JJ, Dodek PM. Risk markers for thrombocytopenia in critically ill patients: a prospective analysis. Pharmacotherapy. 2002. 22:803–813.9. Drews RE, Weinberger SE. Thrombocytopenic disorders in critically ill patients. Am J Respir Crit Care Med. 2000. 162:347–351.10. Fahey VA. Heparin-induced thrombocytopenia. J Vasc Nurs. 1995. 13:112–116.11. Selleng K, Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia in intensive care patients. Crit Care Med. 2007. 35:1165–1176.12. Linkins LA, Dans AL, Moores LK, Bona R, Davidson BL, Schulman S, Crowther M. Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012. 141:e495S–e530S.13. Levi M. Disseminated intravascular coagulation. Crit Care Med. 2007. 35:2191–2195.14. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003. 29:530–538.15. Neame PB, Kelton JG, Walker IR, Stewart IO, Nossel HL, Hirsh J. Thrombocytopenia in septicemia: the role of disseminated intravascular coagulation. Blood. 1980. 56:88–92.16. Stephan F, Thioliere B, Verdy E, Tulliez M. Role of hemophagocytic histiocytosis in the etiology of thrombocytopenia in patients with sepsis syndrome or septic shock. Clin Infect Dis. 1997. 25:1159–1164.17. Priziola JL, Smythe MA, Dager WE. Drug-induced thrombocytopenia in critically ill patients. Crit Care Med. 2010. 38:S145–S154.18. Warkentin TE, Cook RJ, Marder VJ, Sheppard JA, Moore JC, Eriksson BI, Greinacher A, Kelton JG. Anti-platelet factor 4/heparin antibodies in orthopedic surgery patients receiving antithrombotic prophylaxis with fondaparinux or enoxaparin. Blood. 2005. 106:3791–3796.19. Sakr Y. Heparin-induced thrombocytopenia in the ICU: an overview. Crit Care. 2011. 15:211–219.20. Menajovsky LB. Heparin-induced thrombocytopenia: clinical manifestations and management strategies. Am J Med. 2005. 118:Suppl 8A. 21S–30S.21. Greinacher A, Althaus K, Krauel K, Selleng S. Heparin-induced thrombocytopenia. Hamostaseologie. 2010. 30:17–18. 20–28.22. Morel-Kopp MC, Aboud M, Tan CW, Kulathilake C, Ward C. Heparin-induced thrombocytopenia: evaluation of IgG and IgGAM ELISA assays. Int J Lab Hematol. 2011. 33:245–250.23. Sprung CL, Peduzzi PN, Shatney CH, Schein RM, Wilson MF, Sheagren JN, Hinshaw LB. The Veterans Administration Systemic Sepsis Cooperative Study Group. Impact of encephalopathy on mortality in the sepsis syndrome. Crit Care Med. 1990. 18:801–806.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Thrombocytopenia and Changes in Platelet Counts as Prognostic Markers in Pediatric Intensive Care Units
- Rehabilitation in Intensive Care Unit
- Risk Factors of Medical Device-Related Pressure Ulcer in Intensive Care Units
- Risk Factors and Prognosis of Early Onset Thrombocytopenia in Extremely Low Birth Weight Infants
- Causes and Neonatal Outcome of Early-Onset Thrombocytopenia in Preterm Neonates