J Korean Med Sci.
2012 Jul;27(7):794-798. 10.3346/jkms.2012.27.7.794.
Fetal Heart Rate Regresses toward the Mean in the Third Trimester
- Affiliations
-
- 1Department of Mathematics, Research Institute of Natural Sciences, Hanyang University College of Medicine, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Hanyang University College of Medicine, Seoul, Korea. parkmi@hanyang.ac.kr
- KMID: 2157926
- DOI: http://doi.org/10.3346/jkms.2012.27.7.794
Abstract
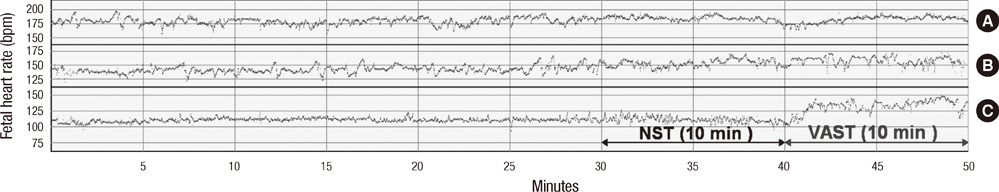
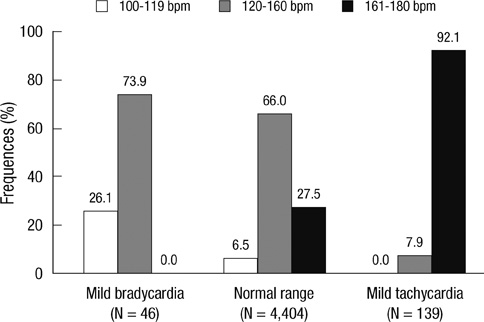
- The purpose of this study was to investigate the feasibility of different fetal heart rate (FHR) ranges in the nonstress test (NST) and to better understand the meaning of mild bradycardia and/or tachycardia without non-reassuring patterns. We employed the heredity to show that mild bradycardia (100-119 beats per minute, bpm) and mild tachycardia (161-180 bpm) regressed to the normal FHR range (120-160 bpm). We used linear regression to analyze FHR data from FHR tracings recorded 10 min before (NST, as the predictor) and 10 min after vibroacoustic stimulation testing (as the dependent variable). Acceleration for 15 bpm-15 seconds (Acc1515) and deceleration for 15 bpm-15 seconds (Dec1515) in the NST were also analyzed for each group. The slope of the best-fit line was the largest in the mild bradycardia group and the smallest in the normal range group. Dec1515 was most prominent in mild tachycardia and both the mild bradycardia and tachycardia groups regressed towards the mean FHR range. Therefore, we propose that both mild bradycardia and tachycardia of FHR in non-acute situations (range between 100 and 180 bpm) are not regarded a pathologic signal for clinical use.
Keyword
MeSH Terms
Figure
Reference
-
1. Manassiev N. What is the normal heart rate of a term fetus? Br J Obstet Gynaecol. 1996. 103:1272–1273.2. Gibb D, Arulkumaran S. Fetal monitoring in practice. 1997. 2nd ed. Oxford: Butterworth Heinmann;20–22.3. Spencer J. Chamberlain G, editor. Anteparturn tocography. Modern antenatal care of the fetus. 1990. Oxford: Blackwell Science Ltd;163–188.4. American College of Obstetricians and Gynecologists. Fetal heart rate patterns: monitoring, interpretation, and management. ACOG Technical Bulletin 207. 1995. Washington, DC: American College of Obstetricians and Gynecologists.5. Sweha A, Hacker TW, Nuovo J. Interpretation of the electronic fetal heart rate during labor. Am Fam Physician. 1999. 59:2487–2500.6. Chan J, Cabrol D, Ingemarsson I, Marsal K, Moutquin JM, Fisk NM. Pragmatic comparison of β2-agonist side effects within the Worldwide Atosiban versus Beta Agonists study. Eur J Obstet Gynecol Reprod Biol. 2006. 128:135–141.7. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. J Obstet Gynecol Neonatal Nurs. 2008. 37:510–515.8. The Royal Australian and New Zealand College of Gynaecologists. Intrapartum fetal surveillance, clinical guidelines. 2006. Melbourne, Victoria: RANZCOG, Australia.9. Devoe LD. Antenatal fetal assessment: contraction stress test, nonstress test, vibroacoustic stimulation, amniotic fluid volume, biophysical profile, and modified biophysical profile: an overview. Semin Perinatol. 2008. 32:247–252.10. Park YJ, Park SH, Kim YJ, Hoh JK, Park YS, Park MI. Computerized fetal heart rate monitoring after vibroacoustic stimulation in the anencephalic fetus. Early Hum Dev. 2010. 86:569–572.11. Hoh JK, Park YS, Cha KJ, Park MI. Fetal heart rate after vibroacoustic stimulation. Int J Gynaecol Obstet. 2009. 106:14–18.12. Bland JM, Altman DG. Regression towards the mean. BMJ. 1994. 308:1499.13. Sebire NJ, Nayar R, Carvalho M, Soares W, Nicolaides KH. Fetal heart rate at 10 to 14 weeks and birthweight. Br J Obstet Gynaecol. 1997. 104:1207–1209.14. Park MI, Hwang JH, Cha KJ, Park YS, Koh SK. Computerized analysis of fetal heart rate parameters by gestational age. Int J Gynaecol Obstet. 2001. 74:157–164.15. Kuo TB, Lai CJ, Huang YT, Yang CC. Regression analysis between heart rate variability and baroreflex-related vagus nerve activity in rats. J Cardiovasc Electrophysiol. 2005. 16:864–869.16. Clemons T. A look at the inheritance of height using regression toward the mean. Hum Biol. 2000. 72:447–454.17. Yang CC, Chao TC, Kuo TB, Yin CS, Chen HI. Preeclamptic pregnancy is associated with increased sympathetic and decreased parasympathetic control of HR. Am J Physiol Heart Circ Physiol. 2000. 278:H1269–H1273.18. Hutson JM, Mueller-Heubach E. Diagnosis and management of intrapartum reflex fetal heart rate changes. Clin Perinatol. 1982. 9:325–337.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Technique of fetal echocardiography
- Significance of fetal heart rate by vaginal ultrasound in the early pregnancy
- Normal Variation and Predictive Value for Pregnancy Outcome of Fetal Heart Rate in the Early First Trimester
- First and Early Second Trimester Diagnosis of Fetal Heart Disease
- Clinical study on fetal heart rate and fetal movement reponse to music sound stimulation