J Korean Med Sci.
2006 Feb;21(1):172-176. 10.3346/jkms.2006.21.1.172.
Giant Vascular Eccrine Spiradenoma: Report of a Case with Immunohistochemical Study
- Affiliations
-
- 1Department of Dermatology, Hanyang University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Hanyang University College of Medicine, Seoul, Korea. parkcg@hanyang.ac.kr
- KMID: 2157804
- DOI: http://doi.org/10.3346/jkms.2006.21.1.172
Abstract
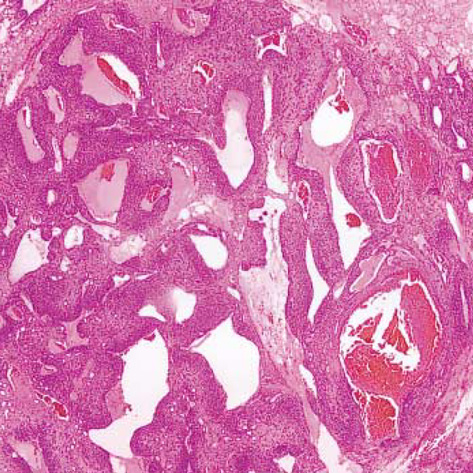
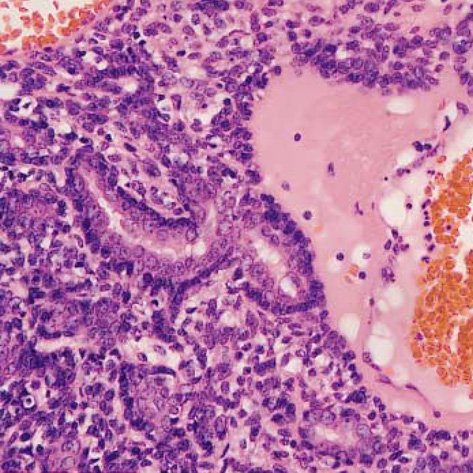
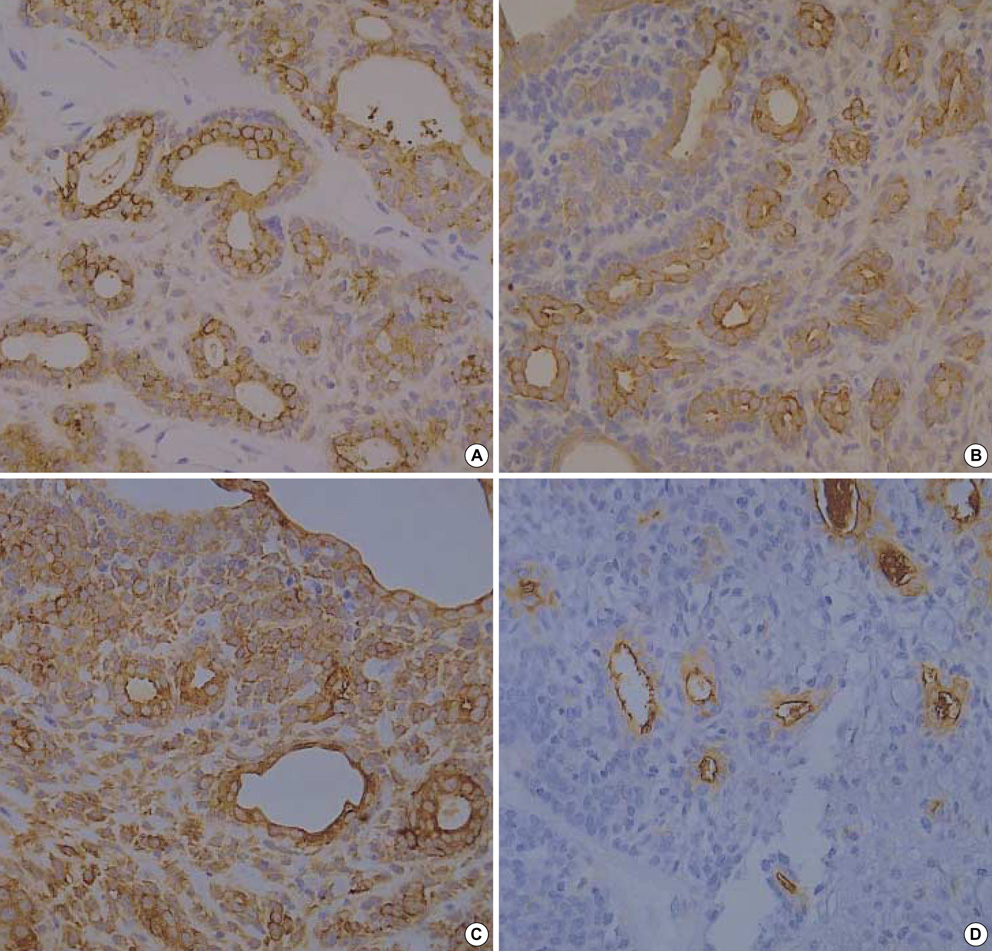
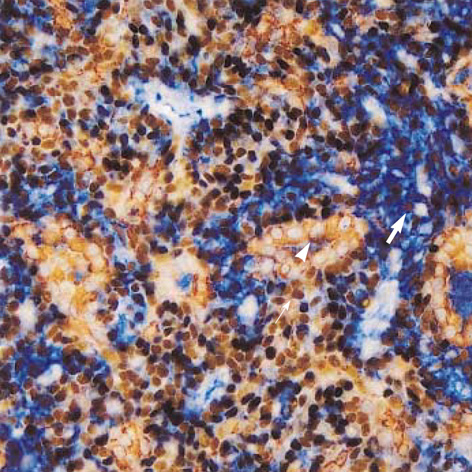
- We report a rare case of giant vascular eccrine spiradenoma (GVES) which developed in 56-yr-old Korean woman. It is a rare variant of eccrine spiradenoma (ES), which might be mistaken for angiomatous lesions in view of its florid vascularity and hemorrhagic features. Histogenesis of GVES is not clearly elucidated although it is known that ES presumably originates in the eccrine glands. To clarify the histogenesis of GVES, immunohistochemical stainings using various monoclonal antibodies were also performed. The tumor was composed of three types of cells, namely pale epithelial cells, small basal cells, and myoepithelial cells. Therefore, we conclude that GVES originated from eccrine gland and mainly differentiates toward secretory portion of secretory coil.
MeSH Terms
-
Actins/analysis
Adenoma, Sweat Gland/blood supply/metabolism/*pathology
Biological Markers/analysis
CA-15-3 Antigen/analysis
Eccrine Glands/blood supply/chemistry/*pathology
Female
Humans
Immunohistochemistry
Keratin/analysis
Korea
Membrane Proteins/analysis
Middle Aged
Muscle, Smooth/chemistry
Sweat Gland Neoplasms/blood supply/metabolism/*pathology
Figure
Cited by 1 articles
-
Giant Vascular Eccrine Spiradenoma
Min Ho Kim, Eujin Cho, Jeong Deuk Lee, Sang Hyun Cho
Ann Dermatol. 2011;23(Suppl 2):S197-S200. doi: 10.5021/ad.2011.23.S2.S197.
Reference
-
1. Cotton DW, Slater DN, Rooney N, Goepel JR, Mills PM. Giant vascular eccrine spiradenomas: a report of two cases with histology, immunohistology and electron microscopy. Histopathology. 1986. 10:1093–1099.
Article2. Hey A, Grouls V, Rockelein G. Vascular eccrine giant spiradenoma-a case report with histology and immunohistology of a rare variant of benign sweat gland tumors. Z Hautkr. 1988. 63:444–447.3. Senol M, Ozcan A, Sasmaz S, Ozen S, Ciralik H. Giant vascular eccrine spiradenoma. Int J Dermatol. 1998. 37:221–223.
Article4. Watanabe S, Hirose M, Sato S, Takahashi H. Immunohistochemical analysis of cytokeratin expression in eccrine spiradenoma: similarities to the transitional portions between secretory segments and coiled ducts of eccrine glands. Br J Dermatol. 1994. 131:799–807.
Article5. Eckert F, Betke M, Schmoeckel C, Neuweiler J, Schmid U. Myoepithelial differentiation in benign sweat gland tumors. Demonstrated by a monoclonal antibody to alpha-smooth muscle actin. J Cutan Pathol. 1992. 19:294–301.
Article6. Maiorana A, Nigrisoli E, Papotti M. Immunohistochemical markers of sweat gland tumors. J Cutan Pathol. 1986. 13:187–196.
Article7. Tsujita-Kyutoku M, Kiuchi K, Danbara N, Yuri T, Senzaki H, Tsubura A. p63 expression in normal human epidermis and epidermal appendages and their tumors. J Cutan Pathol. 2003. 30:11–17.
Article8. Chilosi M, Zamo A, Brighenti A, Malpeli G, Montagna L, Piccoli P, Pedron S, Lestani M, Inghirami G, Scarpa A, Doglioni C, Menestrina F. Constitutive expression of DeltaN-p63alpha isoform in human thymus and thymic epithelial tumours. Virchows Arch. 2003. 443:175–183.9. Krenacs T, Laszik Z, Dobo E. Application of immunogold-silver staining and immunoenzymatic methods in multiple labelling of human pancreatic Langerhans islet cells. Acta Histochem. 1989. 85:79–85.