J Korean Med Sci.
2005 Dec;20(6):1066-1069. 10.3346/jkms.2005.20.6.1066.
Familial Interstitial Lung Disease in Two Young Korean Sisters
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sjhong@amc.seoul.kr
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2157764
- DOI: http://doi.org/10.3346/jkms.2005.20.6.1066
Abstract
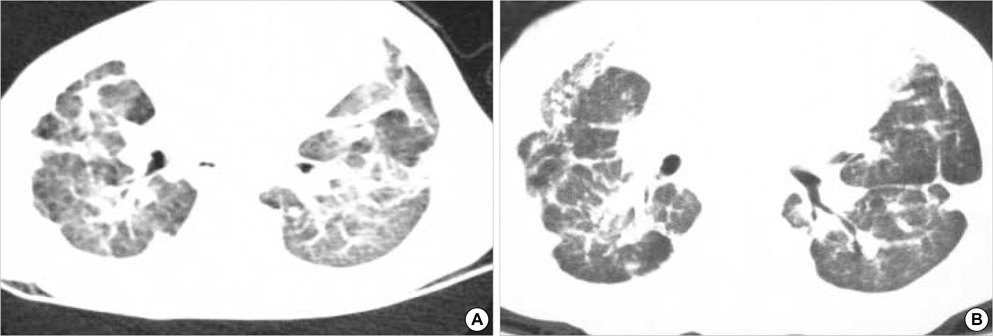
- Most of the interstitial lung diseases are rare, chronic, progressive and fatal disorders, especially in familial form. The etiology of the majority of interstitial lung disease is still unknown. Host susceptibility, genetic and environmental factors may influence clinical expression of each disease. With familial interstitial lung diseases, mutations of surfactant protein B and surfactant protein C or other additional genetic mechanisms (e.g. mutation of the gene for ATP-binding cassette transporter A3) could be associated. We found a 21 month-old girl with respiratory symptoms, abnormal radiographic findings and abnormal open lung biopsy findings compatible with nonspecific interstitial pneumonitis that is similar to those of her older sister died from this disease. We performed genetic studies of the patient and her parents, but we could not find any mutation in our case. High-dose intravenous methylprednisolone and oral hydroxychloroquine were administered and she is still alive without progression during 21 months of follow-up.
MeSH Terms
Figure
Reference
-
1. Balasubramanyan N, Murphy A, O'Sullivan J, O'Connell EJ. Familial interstitial lung disease in children: response to chloroquine treatment in one sibling with desquamative interstitial pneumonitis. Pediatr Pulmonol. 1997. 23:55–61.
Article2. American Thoracic Society and European Respiratory Society. Idiopathic pulmonary fibrosis: diagnosis and treatment. Am J Respir Crit Care Med. 2000. 161:646–664.3. Bitterman PB, Rennard SI, Keogh BA, Wewers MD, Adelberg S, Crystal RG. Familial idiopathic pulmonary fibrosis: evidence of lung inflammation in unaffected family members. N Engl J Med. 1986. 314:1343–1347.4. Amin RS, Wert SE, Baughman RP, Tomashefski JF Jr, Nogee LM, Brody AS, Hull WM, Whitsett JA. Surfactant protein deficiency in familial interstitial lung disease. J Pediatr. 2001. 139:85–92.
Article5. Chernick V. Interstitial lung disease in children: an overview. Pediatr Pulmonol. 1999. 27:Suppl 18. 30s.
Article6. Thomas AQ, Lane K, Phillips J III, Prince M, Markin C, Speer M, Schwartz DA, Gaddipati R, Marney A, Johnson J, Roberts R, Haines J, Stahlman M, Loyd JE. Heterozygosity for a surfactant protein C gene mutation associated with usual interstitial pneumonitis and cellular nonspecific interstitial pneumonitis in one kindred. Am J Respir Crit Care Med. 2002. 165:1322–1328.
Article7. Solliday NH, Williams JA, Gaensler EA, Coutu RE, Carrington CB. Familial chronic interstitial pneumonitis. Am Rev Respir Dis. 1973. 108:193–204.8. Hodgson U, Laitinen T, Tukiainen P. Nationwide prevalence of sporadic and familial idiopathic pulmonary fibrosis: evidence of founder effect among multiplex families in Finland. Thorax. 2002. 57:338–342.
Article9. Verleden GM, du Bois RM, Bouros D, Drent M, Millar A, Müller-Quernheim J, Semenzato G, Johnson S, Sourvino G, Olivier D, Pietinalho A, Xaubet A. Genetic predisposition and pathogenetic mechanisms of interstitial lung disease of unknown origin. Eur Respir J. 2001. 32:17–29.10. Nogee LM, Dunbar AE III, Wert SE, Askin F, Hamvas A, Whitsett JA. A mutation in the surfactant protein C gene associated with familial interstitial lung disease. N Engl J Med. 2001. 344:573–579.
Article11. Whitsett JA, Weaver TE. Hydrophobic surfactant proteins in lung function and disease. N Engl J Med. 2002. 347:2141–2148.
Article12. Fan LL, Kozinetz CA. Factors influencing survival in children with chronic interstitial lung disease. Am J Respir Crit Care Med. 1997. 156:939–942.
Article13. Stern RC. Behrman RE, Kliegman RM, Jenson HB, editors. Idiopathic diffuse interstitial fibrosis of the lung. Nelson's Textbook of Pediatrics. 2003. 16th de. Philadelphia: W.B. Saunders;1299.14. Shulenin S, Nogee LM, Annilo T, Wert SE, Whitsett JA, Dean M. ABCA3 gene mutations in newborns with fatal surfactant deficiency. N Engl J Med. 2004. 350:1296–1303.15. Lee KS, Chung MP. Idiopathic interstitial pneumonias: clinical findings, pathogenesis, pathology and radiologic findings. J Korean Med Sci. 1999. 14:113–127.
Article16. Chung JH, Ha SJ, Kim BS, Hong SJ. Clinical spectrum and lung pathology in children with interstitial lung disease. J Korean Pediatr Soc. 2002. 45:79–87.17. Desmarquest P, Tamalet A, Fauroux B, Boule M, Boccon-Gibod L, Tournier G, Clement A. Chronic interstitial lung disease in children: response to high-dose intravenous methylprednisolone pulses. Pediatr Pulmonol. 1998. 26:332–338.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Interstitial Pneumonias: Radiologic Findings
- Interstitial Lung Diseases: Respiratory Review of 2013
- The Comparision of the Clinical, Laboratory and Radiologic Factors in Rheumatoid Arthritis Patients with or Without Interstitial Lung Disease
- A Radiologic Approach to Diffuse Interstitial Lung Disease
- Pathology of Chronic Interstitial Lung Disease