Ann Dermatol.
2011 Sep;23(Suppl 1):S57-S60. 10.5021/ad.2011.23.S1.S57.
The Three Dimensional Conformal Radiotherapy for Hyperkeratotic Plantar Mycosis Fungoides
- Affiliations
-
- 1Department of Radiation Oncology, Chonbuk National University Medical School, Jeonju, Korea. jskim@jbnu.ac.kr
- 2Department of Dermatology, Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 2156752
- DOI: http://doi.org/10.5021/ad.2011.23.S1.S57
Abstract
- The localized early-stage of Mycosis fungoides (MF) (stage IA-IIA) is usually treated with topical agents, such as nitrogen mustard, steroids, and phototherapy (UVB/PUVA) as first line therapy; response to these initial treatments is usually good. However, hyperkeratotic plantar lesions are clinically rare and have decreased responsiveness to topical agents. For such cases, physicians may consider local radiotherapy. Here, a case of an 18-year-old Korean woman who was treated with three-dimensional conformal radiotherapy (3D-CRT) for hyperkeratotic plantar lesions that were refractory to UVA-1, methotrexate, and topical steroids is reported. Complete remission was attained after radiotherapy. During the one-year follow-up period, there has been no evidence of disease recurrence and no chronic complications have been observed.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
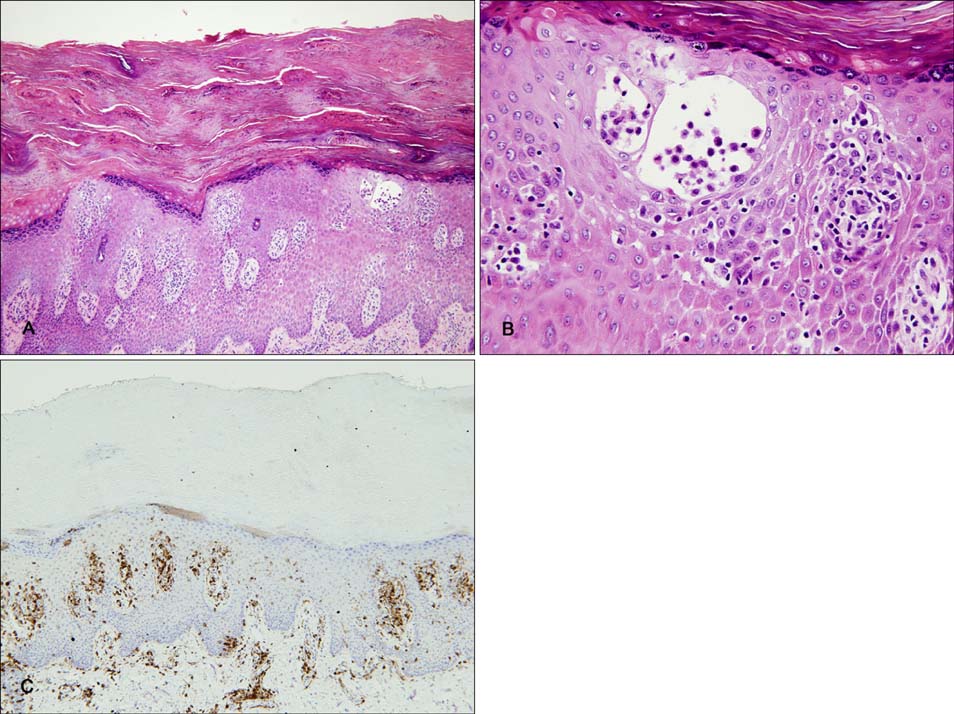
Comment on "Pseudopautrier's Abscess"
Min Soo Jang, Dong Young Kang, Jong Bin Park, Jin Seuk Kang, Sang Tae Kim, Kee Suck Suh
Ann Dermatol. 2012;24(3):376-379. doi: 10.5021/ad.2012.24.3.376.Comment on "Pseudopautrier's Abscess"
Min Soo Jang, Dong Young Kang, Jong Bin Park, Jin Seuk Kang, Sang Tae Kim, Kee Suck Suh
Ann Dermatol. 2012;24(3):376-379. doi: 10.5021/ad.2012.24.3.376.
Reference
-
1. Whittaker SJ, Marsden JR, Spittle M, Russell Jones R. British Association of Dermatologists. U.K. Cutaneous Lymphoma Group. Joint British Association of Dermatologists and U.K. Cutaneous Lymphoma Group guidelines for the management of primary cutaneous T-cell lymphomas. Br J Dermatol. 2003. 149:1095–1107.
Article2. Siegel RS, Pandolfino T, Guitart J, Rosen S, Kuzel TM. Primary cutaneous T-cell lymphoma: review and current concepts. J Clin Oncol. 2000. 18:2908–2925.
Article3. Kneitz H, Bröcker EB, Becker JC. Mycosis fungoides bullosa: a case report and review of the literature. J Med Case Reports. 2010. 4:78.4. Duvic M, Cather J. Emerging new therapies for cutaneous T-cell lymphoma. Dermatol Clin. 2000. 18:147–156.5. Pandya MJ, Rawal RC, Bilimoria FE. Unusual presentation of T-cell lymphoma. Indian J Dermatol Venereol Leprol. 1997. 63:370–372.6. Jacob R, Scala M, Fung MA. A case of syringotropic cutaneous T-cell lymphoma treated with local radiotherapy. J Am Acad Dermatol. 2009. 60:152–154.7. Curt H, Sushil B, Luther WB, Eric CV. Halperin EC, Perez CA, Brady LW, editors. Cutaneous T-cell lymphoma. Perez and Brady's principles and practice of radiation oncology. 2007. 5th ed. Philadelphia: Lippincott Williams & Wilkins;1766–1776.
Article8. Samant RS, Fox GW, Gerig LH, Montgomery LA, Allan DS. Total scalp radiation using image-guided IMRT for progressive cutaneous T-cell lymphoma. Br J Radiol. 2009. 82:e122–e125.
Article9. Eich HT, Eich D, Micke O, Süttzer H, Casper C, Krieg T, et al. Long-term efficacy, curative potential, and prognostic factors of radiotherapy in primary cutaneous B-cell lymphoma. Int J Radiat Oncol Biol Phys. 2003. 55:899–906.10. Purdy JA. Halperin EC, Perez CA, Brady LW, editors. Three-dimensional conformal radiation therapy: physics, treatment planning, and clinical aspects. Perez and Brady's principles and practice of radiation oncology. 2007. 5th ed. Philadelphia: Lippincott Williams & Wilkins;218–238.