Korean J Crit Care Med.
2015 Nov;30(4):323-328. 10.4266/kjccm.2015.30.4.323.
Disseminated Gastrointestinal Mucormycosis in Immunocompromised Disease
- Affiliations
-
- 1Department of Critical Care Medicine, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dr99.park@samsung.com
- 2Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2156189
- DOI: http://doi.org/10.4266/kjccm.2015.30.4.323
Abstract
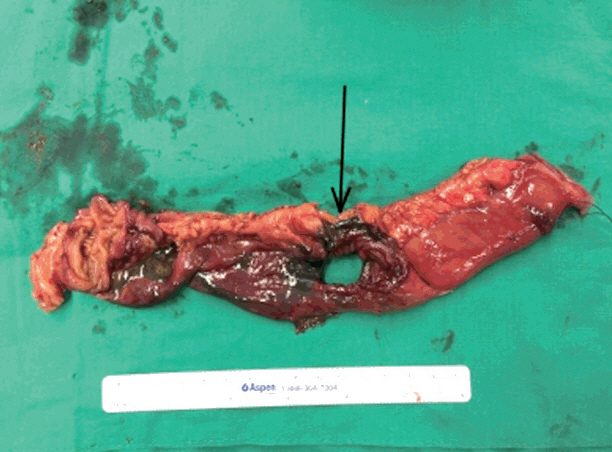
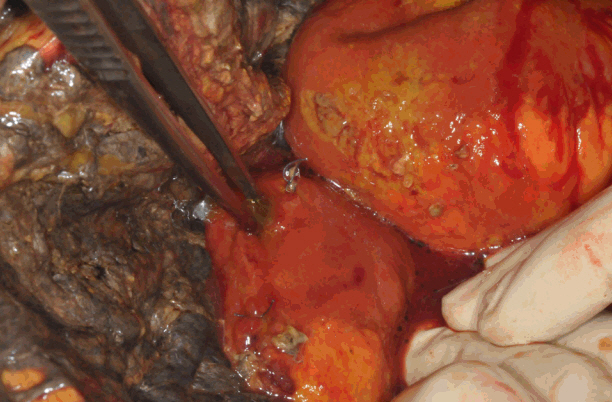
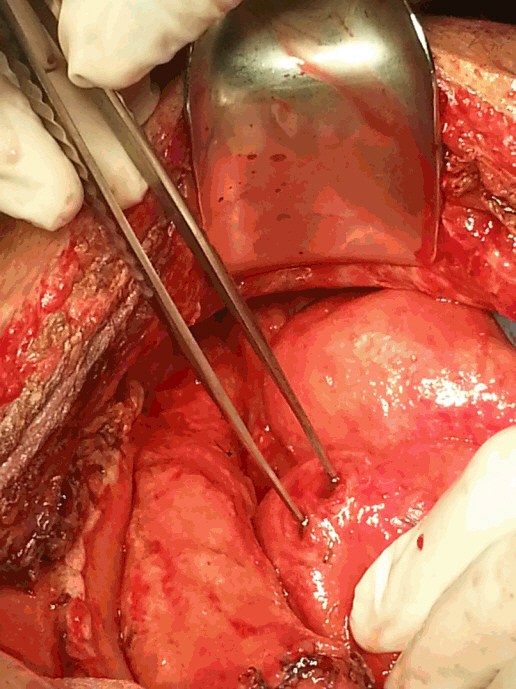
- Mucormycosis is an uncommon opportunistic fungal infection mostly affecting immunocompromised patients and gastrointestinal mucormycosis is a rare and life-threatening. We describe a 31-year-old man with a history of idiopathic cyclic neutropenia who developed perforations of the stomach and intestine and intra-abdominal bleeding due to disseminated gastrointestinal mucormycosis after the initial operation.
MeSH Terms
Figure
Cited by 1 articles
-
Gastric Mucormycosis Followed by Traumatic Cardiac Rupture in an Immunocompetent Patient
Sang Won Lee, Hyun Seok Lee
Korean J Gastroenterol. 2016;68(2):99-103. doi: 10.4166/kjg.2016.68.2.99.
Reference
-
References
1. Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012; 54 Suppl 1:S23–34.
Article2. Gonzalez CE, Rinaldi MG, Sugar AM. Zygomycosis. Infect Dis Clin North Am. 2002; 16:895–914. vi.
Article3. Petrikkos G, Drogari-Apiranthitou M. Zygomycosis in Immunocompromised non-Haematological Patients. Mediterr J Hematol Infect Dis. 2011; 3:e2011012.
Article4. Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect. 2004; 10 Suppl 1:31–47.
Article5. Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000; 13:236–301.
Article6. Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005; 41:634–53.
Article7. Agha FP, Lee HH, Boland CR, Bradley SF. Mucormycoma of the colon: early diagnosis and successful management. AJR Am J Roentgenol. 1985; 145:739–41.
Article8. Lo OS, Law WL. Ileocolonic mucormycosis in adult immunocompromised patients: a surgeon’s perspective. World J Gastroenterol. 2010; 16:1165–70.
Article9. Lee SH, Son YG, Sohn SS, Ryu SW. Successful treatment of invasive gastric mucormycosis in a patient with alcoholic liver cirrhosis: a case report. Exp Ther Med. 2014; 8:401–4.
Article10. Yang YC, Park CK, Kim JS, Park NH, Lee SH, Kim SR, et al. A case of mucormycosis colonization associated with giant gastric ulcer. Korean J Gastrointest Endosc. 2000; 20:49–52.11. Han JY, Cheon JH, Kim DH, Chon HJ, Kim SK, Kim TI, et al. Ileal mucormycosis diagnosed by colonoscopy in a patient with acute myeloid leukemia. Korean J Gastroenterol. 2008; 52:179–82.12. Suh IW, Park CS, Lee MS, Lee JH, Chang MS, Woo JH, et al. Hepatic and small bowel mucormycosis after chemotherapy in a patient with acute lymphocytic leukemia. J Korean Med Sci. 2000; 15:351–4.
Article13. Kontoyiannis DP, Wessel VC, Bodey GP, Rolston KV. Zygomycosis in the 1990s in a tertiary-care cancer center. Clin Infect Dis. 2000; 30:851–6.
Article14. Kontoyiannis DP, Lewis RE. Invasive zygomycosis: update on pathogenesis, clinical manifestations, and management. Infect Dis Clin North Am. 2006; 20:581–607. vi.
Article15. Spellberg B, Walsh TJ, Kontoyiannis DP, Edwards J Jr, Ibrahim AS. Recent advances in the management of mucormycosis: from bench to bedside. Clin Infect Dis. 2009; 48:1743–51.
Article16. Gómez-López A, Cuenca-Estrella M, Monzón A, Rodriguez-Tudela JL. In vitro susceptibility of clinical isolates of Zygomycota to amphotericin B, flucytosine, itraconazole and voriconazole. J Antimicrob Chemother. 2001; 48:919–21.17. van Burik JA, Hare RS, Solomon HF, Corrado ML, Kontoyiannis DP. Posaconazole is effective as salvage therapy in zygomycosis: a retrospective summary of 91 cases. Clin Infect Dis. 2006; 42:e61–5.
Article18. Liles WC, Huang JE, van Burik JA, Bowden RA, Dale DC. Granulocyte colony-stimulating factor administered in vivo augments neutrophil-mediated activity against opportunistic fungal pathogens. J Infect Dis. 1997; 175:1012–5.
Article19. Garcia-Diaz JB, Palau L, Pankey GA. Resolution of rhinocerebral zygomycosis associated with adjuvant administration of granulocyte-macrophage colony-stimulating factor. Clin Infect Dis. 2001; 32:e145–50.
Article20. Vaes M, Hites M, Cotton F, Bourguignon AM, Csergö M, Rasson C, et al. Therapeutic drug monitoring of posaconazole in patients with acute myeloid leukemia or myelodysplastic syndrome. Antimicrob Agents Chemother. 2012; 56:6298–303.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fatal Case of Disseminated Intestinal Mucormycosis in a Patient with Vibrio Sepsis
- A Case of Peritonitis and Disseminated Mucormycosis Caused by Mucor circinelloides in a Patient with Nodal Marginal Zone B-cell Lymphoma
- A Case of Ileal Mucormycosis in a Patient with Gastrointestinal Behcet's Disease
- A Case of Gastric Mucormycosis Associated with Diabetes Mellitus and Alcoholic Hepatitis
- A Case of Disseminated Mucormycosis after Allogenic Bone Marrow Transplantation