Korean J Crit Care Med.
2015 Nov;30(4):313-317. 10.4266/kjccm.2015.30.4.313.
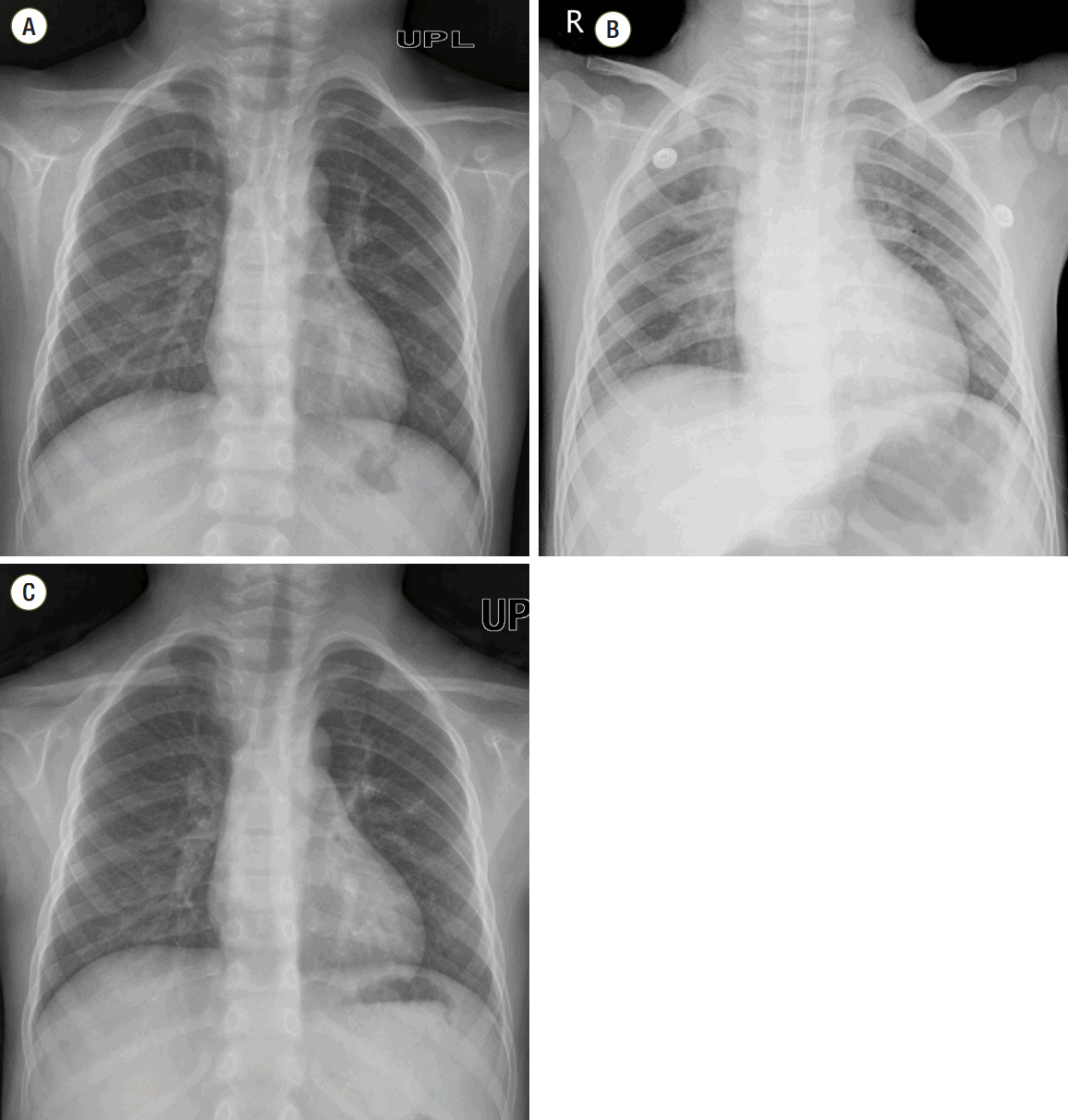
Aspiration Pneumonia in a Pediatric Patient under General Anesthesia despite Adequate Preoperative Fasting
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea. kjm@khnmc.or.kr
- KMID: 2156187
- DOI: http://doi.org/10.4266/kjccm.2015.30.4.313
Abstract
- Aspiration pneumonia rarely occurs during general anesthesia; however, it can result in fatal pulmonary complications. To reduce aspiration pneumonia, a preoperative fasting time of 8 hours is recommended. A 4-year-old boy with ankyloglossia was scheduled for frenotomy. He completed preoperative fasting time and had no digestive symptoms. Pulmonary aspiration due to unexpected massive vomiting occurred during anesthesia induction. The patient's airway was immediately secured by endotracheal tube. The vomitus in the airway tract was removed by fiberoptic bronchoscopy. Abdomen radiograph taken after this event showed paralytic ileus which can cause aspiration of gastric contents. We describe a case of pneumonia caused by aspiration of gastric contents in a pediatric patient who followed fasting instructions and who was scheduled for outpatient surgery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. American Society of Anesthesiologists Committee. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011; 114:495–511.2. Shime N, Ono A, Chihara E, Tanaka Y. Current status of pulmonary aspiration associated with general anesthesia: a nationwide survey in Japan. Masui. 2005; 54:1177–85.3. Lienhart A, Auroy Y, Péquignot F, Benhamou D, Warszawski J, Bovet M, et al. Survey of anesthesia-related mortality in France. Anesthesiology. 2006; 105:1087–97.
Article4. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001; 344:665–71.
Article5. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003; 124:328–36.
Article6. Warner MA, Warner ME, Warner DO, Warner LO, Warner EJ. Perioperative pulmonary aspiration in infants and children. Anesthesiology. 1999; 90:66–71.
Article7. Saunders MD. Acute colonic pseudo-obstruction. Best Pract Res Clin Gastroenterol. 2007; 21:671–87.
Article8. Batke M, Cappell MS. Adynamic ileus and acute colonic pseudo-obstruction. Med Clin North Am. 2008; 92:649–70.
Article9. Camilleri M, Hasler WL, Parkman HP, Quigley EM, Soffer E. Measurement of gastrointestinal motility in the GI laboratory. Gastroenterology. 1998; 115:747–62.
Article10. Vantrappen G. Methods to study gastric emptying. Dig Dis Sci. 1994; 39(12 Suppl):91S–4S.
Article11. Smout A, Horowitz M, Armstrong D. Methods to study gastric emptying. Frontiers in gastric emptying. Dig Dis Sci. 1994; 39(12 Suppl):130S–2S.12. Bolondi L, Bortolotti M, Santi V, Calletti T, Gaiani S, Labò G. Measurement of gastric emptying time by real-time ultrasonography. Gastroenterology. 1985; 89:752–9.
Article13. Van de Putte P, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth. 2014; 113:12–22.
Article14. Sandora TJ, Harper MB. Pneumonia in hospitalized children. Pediatr Clin North Am. 2005; 52:1059–81. viii.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of pulmonary aspiration due to undiagnosed achalasia during induction of general anesthesia - A case report -
- Aspiration Pneumonia at Recovery Room in the Patient Emergency Pelviscopic Salpingectomy, without the Perceptive Sign of Gastric Regurgitation during Perioperative Periods: A case report
- Pneumonia due to aspiration of povidine iodine after induction of general anesthesia -A case report-
- Aspiration Pneumonia after General Anesthesia Using Laryngeal Mask Airway: A case report
- Pulmonary aspiration during anesthetic induction in a patient with laparoscopic adjustable gastric band: A case report