Korean J Radiol.
2015 Aug;16(4):881-888. 10.3348/kjr.2015.16.4.881.
Imaging of Herniated Discs of the Cervical Spine: Inter-Modality Differences between 64-Slice Multidetector CT and 1.5-T MRI
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Bucheon Hospital, Bucheon 420-767, Korea. mj4907@schmc.ac.kr
- 2Department of Radiology, Soonchunhyang University Cheonan Hospital, Cheonan 330-721, Korea.
- 3Department of Radiology, Soonchunhyang University Seoul Hospital, Seoul 140-743, Korea.
- KMID: 2155563
- DOI: http://doi.org/10.3348/kjr.2015.16.4.881
Abstract
OBJECTIVE
To assess inter-modality variability when evaluating cervical intervertebral disc herniation using 64-slice multidetector-row computed tomography (MDCT) and magnetic resonance imaging (MRI).
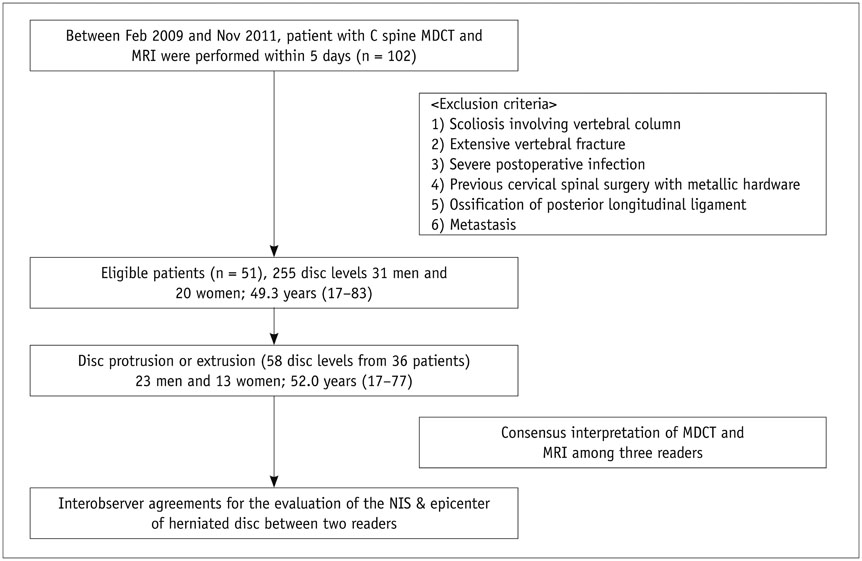
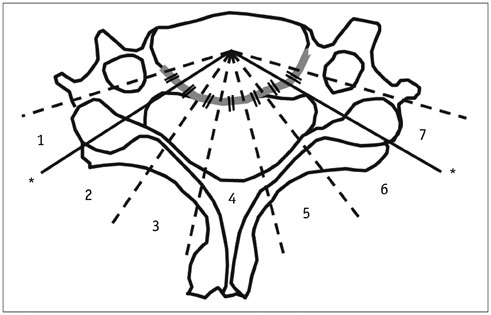
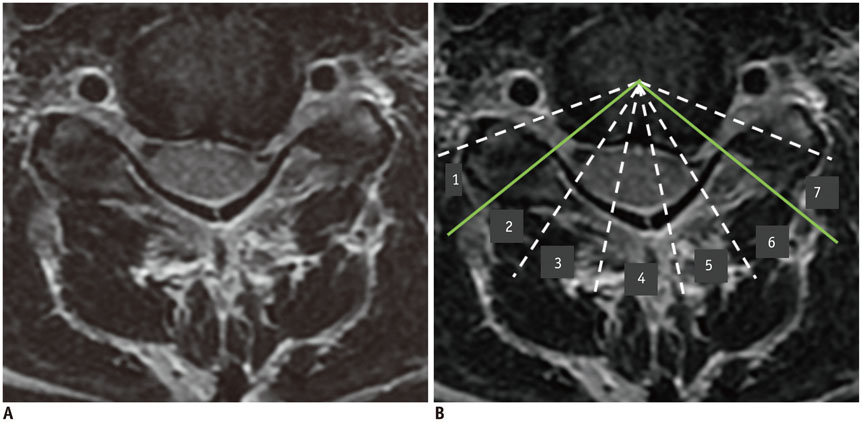
MATERIALS AND METHODS
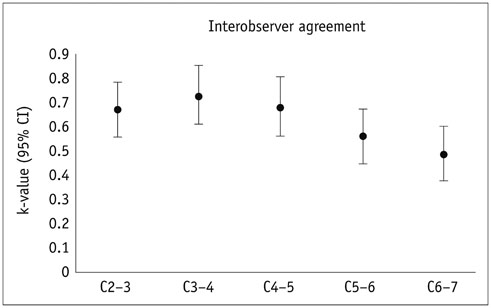
Three musculoskeletal radiologists independently reviewed cervical spine 1.5-T MRI and 64-slice MDCT data on C2-3 though C6-7 of 51 patients in the context of intervertebral disc herniation. Interobserver and inter-modality agreements were expressed as unweighted kappa values. Weighted kappa statistics were used to assess the extents of agreement in terms of the number of involved segments (NIS) in disc herniation and epicenter measurements collected using MDCT and MRI.
RESULTS
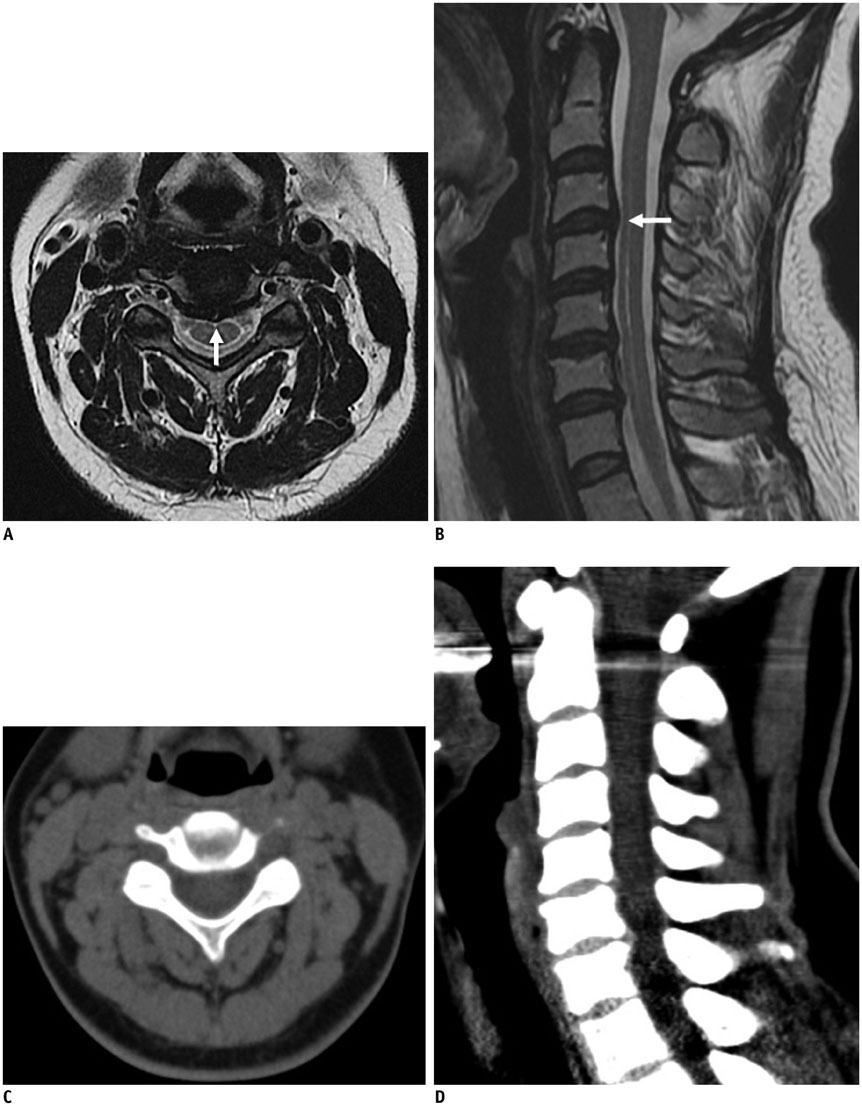
The interobserver agreement rates upon evaluation of disc morphology by the three radiologists were in fair to moderate agreement (k = 0.39-0.53 for MDCT images; k = 0.45-0.56 for MRIs). When the disc morphology was categorized into two and four grades, the inter-modality agreement rates were moderate (k-value, 0.59) and substantial (k-value, 0.66), respectively. The inter-modality agreements for evaluations of the NIS (k-value, 0.78) and the epicenter (k-value, 0.79) were substantial. Also, the interobserver agreements for the NIS (CT; k-value, 0.85 and MRI; k-value, 0.88) and epicenter (CT; k-value, 0.74 and MRI; k-value, 0.70) evaluations by two readers were substantial. MDCT tended to underestimate the extent of herniated disc lesions compared with MRI.
CONCLUSION
Multidetector-row computed tomography and MRI showed a moderate-to-substantial degree of inter-modality agreement for the assessment of herniated cervical discs. MDCT images have a tendency to underestimate the anterior/posterior extent of the herniated disc compared with MRI.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Cervical Spine CT Using Spectral Shaping: Can It Be a Solution to Overcome Artifacts in the Lower Cervical Spinal Region?
Su Min Lee, Hye Jung Choo, Sun Joo Lee, Sung-Kwan Kim, In Sook Lee, Dong Wook Kim, Jin Wook Baek, Young Jin Heo
Korean J Radiol. 2019;20(3):469-478. doi: 10.3348/kjr.2018.0517.
Reference
-
1. Lunsford LD, Bissonette DJ, Jannetta PJ, Sheptak PE, Zorub DS. Anterior surgery for cervical disc disease. Part 1: Treatment of lateral cervical disc herniation in 253 cases. J Neurosurg. 1980; 53:1–11.2. Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994; 117(Pt 2):325–335.3. Daniels DL, Grogan JP, Johansen JG, Meyer GA, Williams AL, Haughton VM. Cervical radiculopathy: computed tomography and myelography compared. Radiology. 1984; 151:109–113.4. Shim JH, Park CK, Lee JH, Choi JW, Lee DC, Kim DH, et al. A comparison of angled sagittal MRI and conventional MRI in the diagnosis of herniated disc and stenosis in the cervical foramen. Eur Spine J. 2009; 18:1109–1116.5. Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC. Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech. 2008; 21:288–292.6. Yousem DM, Atlas SW, Hackney DB. Cervical spine disk herniation: comparison of CT and 3DFT gradient echo MR scans. J Comput Assist Tomogr. 1992; 16:345–351.7. Douglas-Akinwande AC, Rydberg J, Shah MV, Phillips MD, Caldemeyer KS, Lurito JT, et al. Accuracy of contrast-enhanced MDCT and MRI for identifying the severity and cause of neural foraminal stenosis in cervical radiculopathy: a prospective study. AJR Am J Roentgenol. 2010; 194:55–61.8. Larsson EM, Holtås S, Cronqvist S, Brandt L. Comparison of myelography, CT myelography and magnetic resonance imaging in cervical spondylosis and disk herniation. Pre- and postoperative findings. Acta Radiol. 1989; 30:233–239.9. Hudgins WR. Computer-aided diagnosis of lumbar disc herniation. Spine (Phila Pa 1976). 1983; 8:604–615.10. Modic MT, Masaryk T, Boumphrey F, Goormastic M, Bell G. Lumbar herniated disk disease and canal stenosis: prospective evaluation by surface coil MR, CT, and myelography. AJR Am J Roentgenol. 1986; 147:757–765.11. Thornbury JR, Fryback DG, Turski PA, Javid MJ, McDonald JV, Beinlich BR, et al. Disk-caused nerve compression in patients with acute low-back pain: diagnosis with MR, CT myelography, and plain CT. Radiology. 1993; 186:731–738.12. Dorwart RH, LaMasters DL. Applications of computed tomographic scanning of the cervical spine. Orthop Clin North Am. 1985; 16:381–393.13. Wilson DW, Pezzuti RT, Place JN. Magnetic resonance imaging in the preoperative evaluation of cervical radiculopathy. Neurosurgery. 1991; 28:175–179.14. Fardon DF, Milette PC; Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976). 2001; 26:E93–E113.15. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.16. van Rijn JC, Klemetso N, Reitsma JB, Bossuyt PM, Hulsmans FJ, Peul WC, et al. Observer variation in the evaluation of lumbar herniated discs and root compression: spiral CT compared with MRI. Br J Radiol. 2006; 79:372–377.17. Kane AG, Reilly KC, Murphy TF. Swimmer's CT: improved imaging of the lower neck and thoracic inlet. AJNR Am J Neuroradiol. 2004; 25:859–862.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Study of the Open Discectomy of the Herniated Lumbar Disc: Analysis of Relationship between Operative Indications and MRI Findings
- CT-Discography: Diagnostic Accuracy in Lumbar Disc Herniation and Significance of Induced Pain During Procedure
- Retrospective Outcome Evaluation of Cervical Chemonucleolysis with Digital Infrared Thermographic Imaging
- Neurological Changes after Closed Reduction of Cervical Spine Injury Using Skull Traction
- Spontaneous Regression of a Radiculopathic Cervical Herniated Disc following Non-surgical Treatment: 3 case reports