Korean J Radiol.
2015 Aug;16(4):846-852. 10.3348/kjr.2015.16.4.846.
Multiparametric Magnetic Resonance Imaging Characteristics of Prostate Tuberculosis
- Affiliations
-
- 1Department of Radiology, Tianjin First Central Hospital, Tianjin 300192, China. shenwen66happy@163.com
- KMID: 2155558
- DOI: http://doi.org/10.3348/kjr.2015.16.4.846
Abstract
OBJECTIVE
To describe the multiparametric magnetic resonance imaging (MRI) appearance of prostate tuberculosis.
MATERIALS AND METHODS
Six patients with prostate tuberculosis were analyzed retrospectively. The mean age of the patients was 60.5 years (range, 48-67 years). The mean prostate specific antigen concentration was 6.62 ng/mL (range, 0.54-14.57 ng/mL). All patients underwent a multiparametric MRI examination.
RESULTS
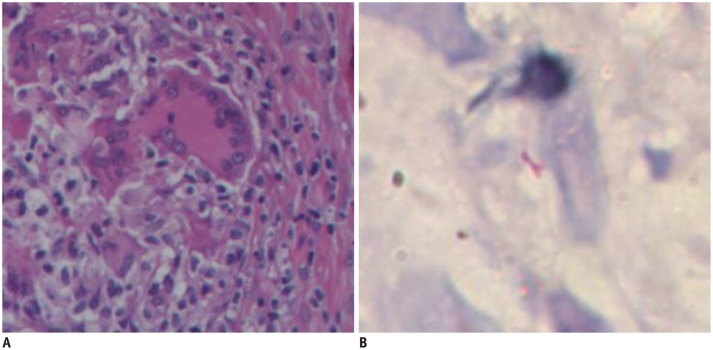
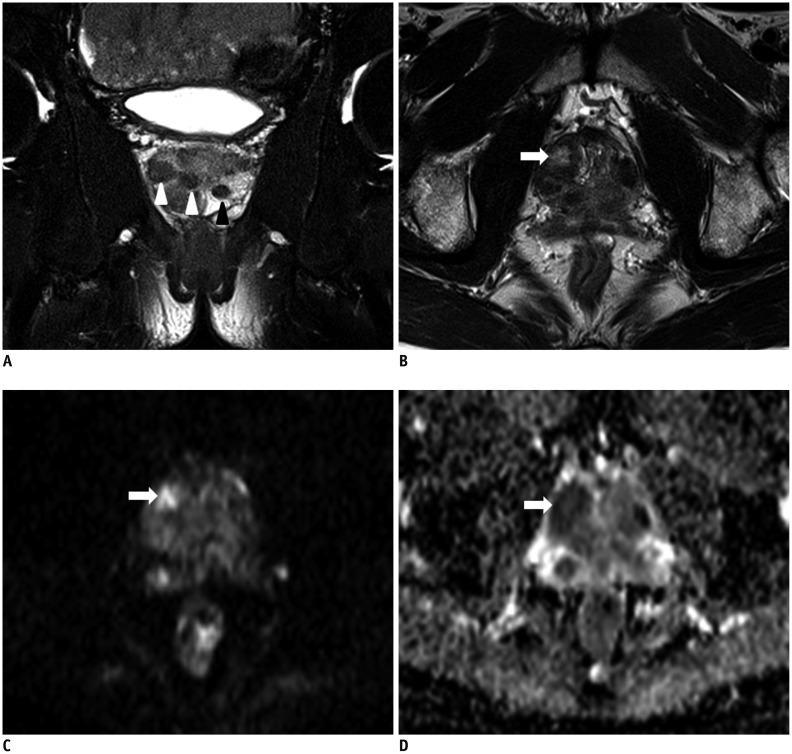
The histopathological results were obtained from biopsies in four men and from transurethral resection of the prostate in two men after the MRI examination. Nodular (33%, 2/6 patients) and diffuse lesions (67%, 4/6 patients) were seen on MRI. The nodular lesions were featured by extremely low signal intensity (similar to that of muscle) on T2-weighted imaging (T2WI). The T2WI signal intensity of the diffuse lesions was low but higher than that of muscle, which showed high signal intensity on diffusion weighted imaging and low signal intensity on an apparent diffusion coefficient map. MR spectroscopic imaging of this type showed a normal-like spectrum. Abscesses were found in one patient with the nodular type and in one with the diffuse type.
CONCLUSION
The appearance of prostate tuberculosis on MRI can be separated into multiple nodular and diffuse types. Multiparametric MRI may offer useful information for diagnosing prostate tuberculosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Chen Y, Liu M, Guo Y. Proton magnetic resonance spectroscopy in prostate tuberculosis. Urology. 2010; 75:1065–1066. PMID: 19781746.
Article2. Suzuki T, Takeuchi M, Naiki T, Kawai N, Kohri K, Hara M, et al. MRI findings of granulomatous prostatitis developing after intravesical Bacillus Calmette-Guérin therapy. Clin Radiol. 2013; 68:595–599. PMID: 23384503.
Article3. Ma W, Kang SK, Hricak H, Gerst SR, Zhang J. Imaging appearance of granulomatous disease after intravesical Bacille Calmette-Guerin (BCG) treatment of bladder carcinoma. AJR Am J Roentgenol. 2009; 192:1494–1500. PMID: 19457810.4. Bour L, Schull A, Delongchamps NB, Beuvon F, Muradyan N, Legmann P, et al. Multiparametric MRI features of granulomatous prostatitis and tubercular prostate abscess. Diagn Interv Imaging. 2013; 94:84–90. PMID: 23079151.
Article5. Sáenz-Abad D, Letona-Carbajo S, Benito-Arévalo JL, Sanioaquín-Conde I, Ruiz-Ruiz FJ. Prostatic tuberculosis: case report. Sao Paulo Med J. 2008; 126:227–228. PMID: 18853033.
Article6. Kostakopoulos A, Economou G, Picramenos D, Macrichoritis C, Tekerlekis P, Kalliakmanis N. Tuberculosis of the prostate. Int Urol Nephrol. 1998; 30:153–157. PMID: 9607885.
Article7. López Barón E, Gómez-Arbeláez D, Díaz-Pérez JA. [Primary prostatic tuberculosis. Case report and bibliographic review]. Arch Esp Urol. 2009; 62:309–313. PMID: 19717881.8. Ludwig M, Velcovsky HG, Weidner W. Tuberculous epididymoorchitis and prostatitis: a case report. Andrologia. 2008; 40:81–83. PMID: 18336455.
Article9. Wang JH, Sheu MH, Lee RC. Tuberculosis of the prostate: MR appearance. J Comput Assist Tomogr. 1997; 21:639–640. PMID: 9216775.10. Chung MH, Lee HG, Kwon SS, Park SH. MR imaging of solitary pulmonary lesion: emphasis on tuberculomas and comparison with tumors. J Magn Reson Imaging. 2000; 11:629–637. PMID: 10862062.
Article11. Kurhanewicz J, Vigneron DB, Hricak H, Narayan P, Carroll P, Nelson SJ. Three-dimensional H-1 MR spectroscopic imaging of the in situ human prostate with high (0.24-0.7-cm3) spatial resolution. Radiology. 1996; 198:795–805. PMID: 8628874.
Article12. Caulier P, Yombi JC, Dufaux M, Feyaerts A, Abi AA, Hainaut P. Prostate abscess following intravesical BCG therapy. Acta Clin Belg. 2009; 64:436–437. PMID: 19999393.
Article13. Aust TR, Massey JA. Tubercular prostatic abscess as a complication of intravesical bacillus Calmette-Guérin immunotherapy. Int J Urol. 2005; 12:920–921. PMID: 16323989.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiparametric MRI in the Detection of Clinically Significant Prostate Cancer
- Prostate Imaging Reporting and Data System (PI-RADS) v 2.1: Overview and Critical Points
- The Use of Magnetic Resonance Imaging in the Prostate Cancer Primary Diagnostic Pathway: Is It Ready for Primetime?
- Are we ready to adopt the European Association of Urology recommendations on multiparametric magnetic resonance imaging in the early detection of prostate cancer?
- Multiparametric magnetic resonance imaging for prostate cancer: A review and update for urologists