Korean J Urol.
2015 Apr;56(4):288-294. 10.4111/kju.2015.56.4.288.
Prevalence and clinical significance of incidental 18F-fluoro-2-deoxyglucose uptake in prostate
- Affiliations
-
- 1Department of Urology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 2Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. cskim@amc.seoul.kr
- KMID: 2155304
- DOI: http://doi.org/10.4111/kju.2015.56.4.288
Abstract
- PURPOSE
To investigate the prevalence and clinical significance of incidental prostate fluoro-2-deoxyglucose (FDG) uptake and to evaluate its impact on patient management.
MATERIALS AND METHODS
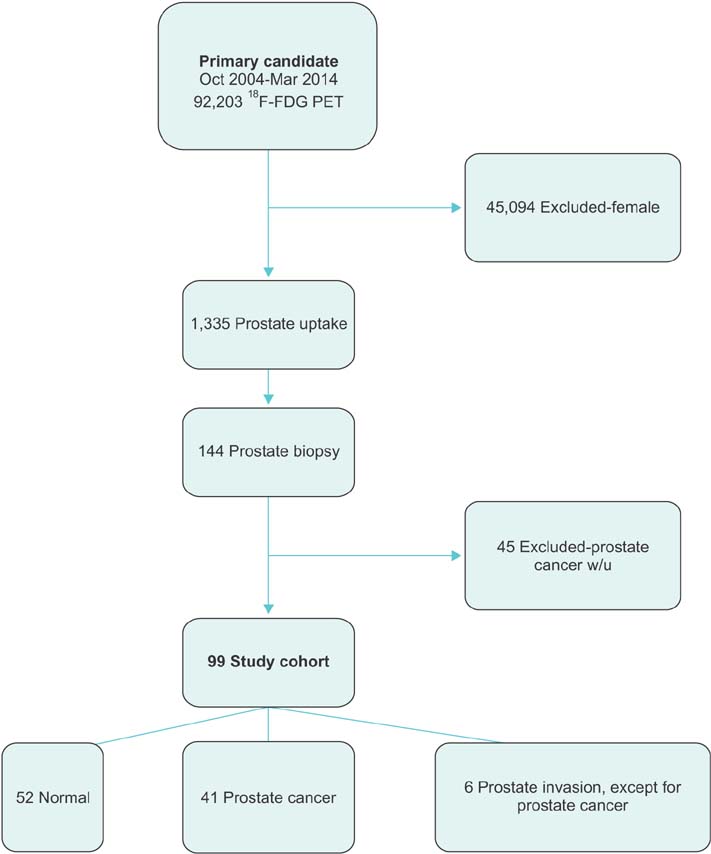
Of 47,109 men who underwent FDG positron emission tomography between 2004 and 2014, 1,335 (2.83%) demonstrated incidental FDG uptake in the prostate, with 99 of the latter undergoing prostate biopsy. The primary end point was the histological presence of prostate adenocarcinoma in the biopsy specimen. Outcomes, including treatment methods, survival, and causes of death, were also assessed. Factors associated with the diagnosis of prostate cancer were evaluated by using logistic regression analysis.
RESULTS
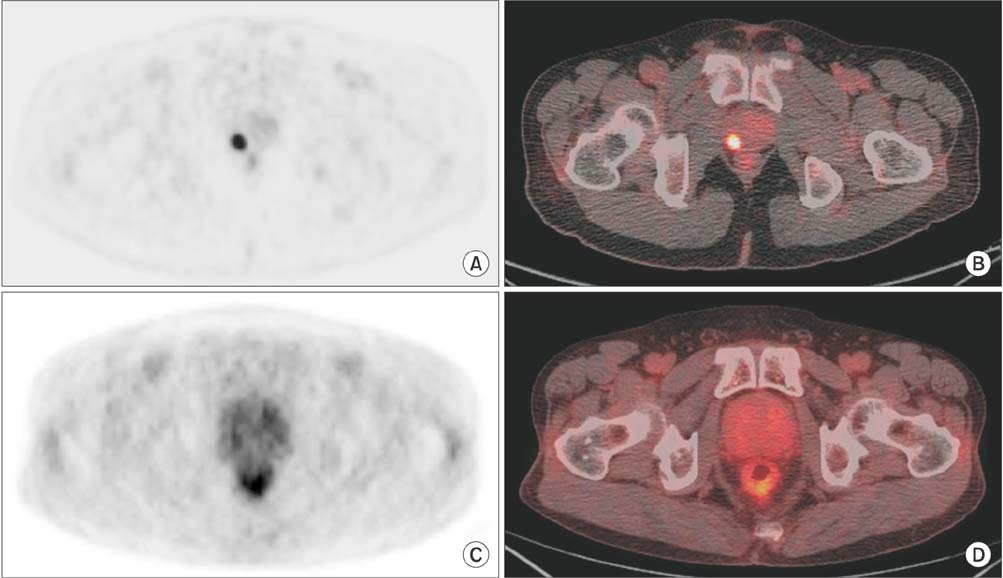
Patients with prostate cancer were more likely to have higher serum prostate-specific antigen (PSA) (p=0.001) and focal FDG uptake (p=0.036) than were those without. Prostate cancer occurred in 1 of 26 patients (3.8%) with serum PSA<2.5 ng/mL, compared with 40 of 67 patients (59.7%) with serum PSA> or =2.5 ng/mL. Multivariable analysis showed that focal lesions (odds ratio [OR], 5.50; p=0.038), age (OR, 1.06; p=0.031), and serum PSA (OR, 1.28; p=0.001) were independent predictors of prostate cancer diagnosis. Most patients with prostate cancer had organ-confined tumors. Of these, 12 (29.3%) underwent radical prostatectomy and 25 (60.9%) received hormone therapy. Of the 11 patients who died, 9 died of primary cancer progression, with only 1 patient dying from prostate cancer.
CONCLUSIONS
The prevalence of incidental FDG uptake in the prostate was not high, although patients with elevated serum PSA had a higher incidence of prostate cancer. Patients with FDG uptake in the prostate should be secondarily evaluated by measuring serum PSA, with those having high serum PSA undergoing prostate biopsy.
MeSH Terms
-
*Adenocarcinoma/epidemiology/pathology/surgery
Aged
Biopsy
Fluorodeoxyglucose F18/*pharmacokinetics
Humans
Incidental Findings
Male
Middle Aged
Organ Specificity
Positron-Emission Tomography/*adverse effects
Prevalence
*Prostate/drug effects/pathology
Prostatectomy/methods/statistics & numerical data
*Prostatic Neoplasms/epidemiology/pathology/surgery
Radiopharmaceuticals/pharmacokinetics
Republic of Korea/epidemiology
Retrospective Studies
Tissue Distribution
Fluorodeoxyglucose F18
Radiopharmaceuticals
Figure
Reference
-
1. Han EJ, O JH, Choi WH, Yoo IR, Chung SK. Significance of incidental focal uptake in prostate on 18-fluoro-2-deoxyglucose positron emission tomography CT images. Br J Radiol. 2010; 83:915–920.2. Facey K, Bradbury I, Laking G, Payne E. Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers. Health Technol Assess. 2007; 11:iii–iv. xi–267.3. Gambhir SS. Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer. 2002; 2:683–693.4. Schaaf WE Jr, Patel Z, Retrouvey M, Cunningham TD, Johnson LS. Frequency and clinical relevance of PET/CT incidentalomas. Abdom Imaging. 2014; 39:657–662.5. Nayan S, Ramakrishna J, Gupta MK. The proportion of malignancy in incidental thyroid lesions on 18-FDG PET study: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2014; 151:190–200.6. Hwang I, Chong A, Jung SI, Hwang EC, Kim SO, Kang TW, et al. Is further evaluation needed for incidental focal uptake in the prostate in 18-fluoro-2-deoxyglucose positron emission tomography-computed tomography images? Ann Nucl Med. 2013; 27:140–145.7. Kao PF, Chou YH, Lai CW. Diffuse FDG uptake in acute prostatitis. Clin Nucl Med. 2008; 33:308–310.8. Takahashi N, Inoue T, Lee J, Yamaguchi T, Shizukuishi K. The roles of PET and PET/CT in the diagnosis and management of prostate cancer. Oncology. 2007; 72:226–233.9. Hyun SH, Choi JY, Lee KH, Choe YS, Kim BT. Incidental focal 18F-FDG uptake in the pituitary gland: clinical significance and differential diagnostic criteria. J Nucl Med. 2011; 52:547–550.10. Leon X, Ferlito A, Myer CM 3rd, Saffiotti U, Shaha AR, Bradley PJ, et al. Second primary tumors in head and neck cancer patients. Acta Otolaryngol. 2002; 122:765–778.11. Lim JH, You D, Jeong IG, Hong JH, Ahn H, Kim CS. Prognosis of prostate cancer with other primary malignancies. Korean J Urol. 2014; 55:327–334.12. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med. 2004; 350:2239–2246.13. Oesterling JE, Jacobsen SJ, Chute CG, Guess HA, Girman CJ, Panser LA, et al. Serum prostate-specific antigen in a community-based population of healthy men. Establishment of agespecific reference ranges. JAMA. 1993; 270:860–864.14. Kumar R, Zhuang H, Alavi A. PET in the management of urologic malignancies. Radiol Clin North Am. 2004; 42:1141–1153.15. Liu IJ, Zafar MB, Lai YH, Segall GM, Terris MK. Fluorodeoxyglucose positron emission tomography studies in diagnosis and staging of clinically organ-confined prostate cancer. Urology. 2001; 57:108–111.16. Oyama N, Akino H, Suzuki Y, Kanamaru H, Sadato N, Yonekura Y, et al. The increased accumulation of [18F]fluorodeoxyglucose in untreated prostate cancer. Jpn J Clin Oncol. 1999; 29:623–629.17. Dong A, Bai Y, Wang Y, Zuo C, Lu J. Spectrum of the prostate lesions with increased FDG uptake on (18)F-FDG PET/CT. Abdom Imaging. 2014; 39:908–921.18. Effert P, Beniers AJ, Tamimi Y, Handt S, Jakse G. Expression of glucose transporter 1 (Glut-1) in cell lines and clinical specimens from human prostate adenocarcinoma. Anticancer Res. 2004; 24(5A):3057–3063.19. Yang Z, Hu S, Cheng J, Xu J, Shi W, Zhu B, et al. Prevalence and risk of cancer of incidental uptake in prostate identified by fluorine-18 fluorodeoxyglucose positron emission tomography/ computed tomography. Clin Imaging. 2014; 38:470–474.20. Untergasser G, Madersbacher S, Berger P. Benign prostatic hyperplasia: age-related tissue-remodeling. Exp Gerontol. 2005; 40:121–128.21. McNeal JE. The zonal anatomy of the prostate. Prostate. 1981; 2:35–49.22. Lee HY, Jeong JY, Lee KS, Kim HJ, Han J, Kim BT, et al. Solitary pulmonary nodular lung adenocarcinoma: correlation of histopathologic scoring and patient survival with imaging biomarkers. Radiology. 2012; 264:884–893.23. Oyama N, Akino H, Kanamaru H, Okada K. Fluorodeoxyglucose positron emission tomography in diagnosis of untreated prostate cancer. Nihon Rinsho. 1998; 56:2052–2055.24. Reynolds MA, Kastury K, Groskopf J, Schalken JA, Rittenhouse H. Molecular markers for prostate cancer. Cancer Lett. 2007; 249:5–13.25. Kazzazi A, Momtahen S, Bruhn A, Hemani M, Ramaswamy K, Djavan B. New findings in localized and advanced prostate cancer: AUA 2011 review. Can J Urol. 2011; 18:5683–5688.26. Carter HB. American Urological Association (AUA) guideline on prostate cancer detection: process and rationale. BJU Int. 2013; 112:543–547.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidental Focal 18F-FDG Uptake in the Prostate: Clinical Significance and Differential Diagnostic Criteria
- Effectiveness of 18F-fluoro-deoxyglucose Positron Emission Tomography/Computed Tomography and Magnetic Resonance Imaging to Detect Iliopsoas Tendonitis after Total Hip Arthroplasty: A Case Report
- Role of 18F 2-fluoro-2-deoxyglucose Positron Emission Tomography in Upper Gastrointestinal Malignancies
- Perirenal 18F-FDG Uptake in a Patient with a Pheochromocytoma
- Clinical Meaning of Incidental Thyroid Uptake on F-18 FDG PET-CT