Ann Rehabil Med.
2016 Feb;40(1):88-94. 10.5535/arm.2016.40.1.88.
The Relation Between the Presence of Aspiration or Penetration and the Clinical Indicators of Dysphagia in Poststroke Survivors
- Affiliations
-
- 1Division of Speech Pathology and Audiology, Hallym University, Chuncheon, Korea.
- 2Department of Physical Medicine and Rehabilitation, Hallym University Medical Center, Chuncheon, Korea.
- 3Communication Sciences and Disorders, Illinois State University, Normal, IL, USA.
- 4Communication Sciences and Disorders, Ohio University, Athens, OH, USA. kimy2@ohio.edu
- KMID: 2155170
- DOI: http://doi.org/10.5535/arm.2016.40.1.88
Abstract
OBJECTIVE
To examine the relation between the presence of penetration or aspiration and the occurrence of the clinical indicators of dysphagia. The presence of penetration or aspiration is closely related to the clinical indicators of dysphagia. It is essential to understand these relationships in order to implement proper diagnosis and treatment of dysphagia.
METHODS
Fifty-eight poststroke survivors were divided into two groups: patients with or without penetration or aspiration. Medical records and videofluoroscopic swallowing examinations were reviewed. The occurrence of clinical indicators of dysphagia between two groups was analyzed with Cross Tabulation and the Pearson chi-square test (p<0.05).
RESULTS
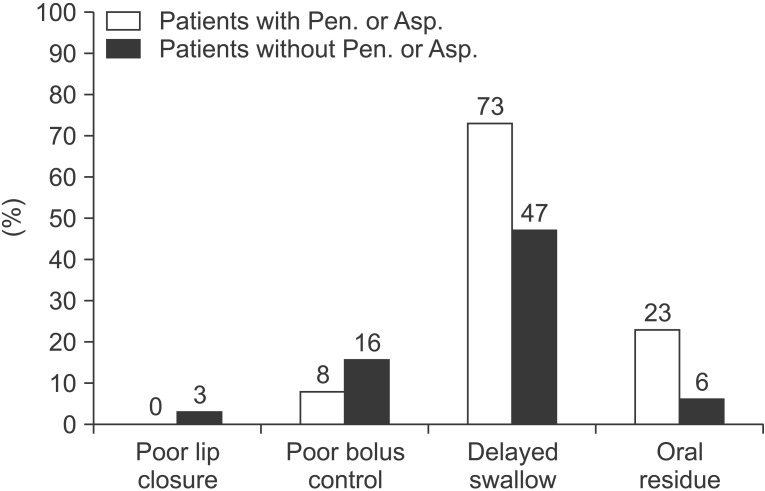
Poststroke survivors with penetration or aspiration had significantly high occurrences of delayed initiation of the swallow (p=0.04) and reduced hyolaryngeal elevation (p<0.01) than those without penetration or aspiration.
CONCLUSION
The results of this study indicate that delayed initiation of the swallow is a strong physiological indicator of penetration or aspiration during the oral stage of swallowing in poststroke survivors. For the pharyngeal stage of swallowing, hyoid and laryngeal elevation is a key event related to occurrence of penetration or aspiration. Clinical indicators should be investigated further to allow appropriate implementation of treatment strategies for stroke survivors.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Lesion Characteristics of Chronic Dysphagia in Patients With Supratentorial Stroke
Sol Jang, Hea Eun Yang, Hee Seung Yang, Dae Hyun Kim
Ann Rehabil Med. 2017;41(2):225-230. doi: 10.5535/arm.2017.41.2.225.Association of Brain Lesions and Videofluoroscopic Dysphagia Scale Parameters on Patients With Acute Cerebral Infarctions
Sang Jun Mo, Ho Joong Jeong, Yong Hyun Han, Kihun Hwang, Jong Kyoung Choi
Ann Rehabil Med. 2018;42(4):560-568. doi: 10.5535/arm.2018.42.4.560.
Reference
-
1. Kidd D, Lawson J, Nesbitt R, MacMahon J. Aspiration in acute stroke: a clinical study with videofluoroscopy. Q J Med. 1993; 86:825–829. PMID: 8108539.2. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.3. Finegold SM. Aspiration pneumonia. Semin Respir Crit Care Med. 1995; 16:475–483.
Article4. Crausaz FM, Favez G. Aspiration of solid food particles into lungs of patients with gastroesophageal reflux and chronic bronchial disease. Chest. 1988; 93:376–378. PMID: 3338306.
Article5. Mann G, Hankey GJ. Initial clinical and demographic predictors of swallowing impairment following acute stroke. Dysphagia. 2001; 16:208–215. PMID: 11453569.
Article6. Power ML, Hamdy S, Singh S, Tyrrell PJ, Turnbull I, Thompson DG. Deglutitive laryngeal closure in stroke patients. J Neurol Neurosurg Psychiatry. 2007; 78:141–146. PMID: 17012336.
Article7. Robbins J, Levin RL. Swallowing after unilateral stroke of the cerebral cortex: preliminary experience. Dysphagia. 1988; 3:11–17. PMID: 3248391.
Article8. Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993; 74:1295–1300. PMID: 8259895.
Article9. Perlman AL, VanDaele DJ, Otterbacher MS. Quantitative assessment of hyoid bone displacement from video images during swallowing. J Speech Hear Res. 1995; 38:579–585. PMID: 7674650.
Article10. Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, et al. Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia. 1989; 4:8–15. PMID: 2640180.
Article11. Perlman AL, Grayhack JP, Booth BM. The relationship of vallecular residue to oral involvement, reduced hyoid elevation, and epiglottic function. J Speech Hear Res. 1992; 35:734–741. PMID: 1405528.
Article12. Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000; 43:1264–1274. PMID: 11063246.
Article13. Perlman AL, Booth BM, Grayhack JP. Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia. 1994; 9:90–95. PMID: 8005013.
Article14. Daniels SK, Schroeder MF, McClain M, Corey DM, Rosenbek JC, Foundas AL. Dysphagia in stroke: development of a standard method to examine swallowing recovery. J Rehabil Res Dev. 2006; 43:347–356. PMID: 17041820.
Article15. Miller JL, Watkin KL. The influence of bolus volume and viscosity on anterior lingual force during the oral stage of swallowing. Dysphagia. 1996; 11:117–124. PMID: 8721070.
Article16. Reddy NP, Thomas R, Canilang EP, Casterline J. Toward classification of dysphagic patients using biomechanical measurements. J Rehabil Res Dev. 1994; 31:335–344. PMID: 7869281.17. Terre R, Mearin F. Oropharyngeal dysphagia after the acute phase of stroke: predictors of aspiration. Neurogastroenterol Motil. 2006; 18:200–205. PMID: 16487410.
Article18. Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998; 13:69–81. PMID: 9513300.
Article19. Logemann JA. Evaluation and treatment of swallowing disorders. Austin: Pro-Ed;1998.20. Cichero JA, Murdoch BE. Dysphagia: foundation, theory, and practice. New York: John Wiley & Sons;2006.21. Ickenstein GW, Stein J, Ambrosi D, Goldstein R, Horn M, Bogdahn U. Predictors of survival after severe dysphagic stroke. J Neurol. 2005; 252:1510–1516. PMID: 16136260.
Article22. Mari F, Matei M, Ceravolo MG, Pisani A, Montesi A, Provinciali L. Predictive value of clinical indices in detecting aspiration in patients with neurological disorders. J Neurol Neurosurg Psychiatry. 1997; 63:456–460. PMID: 9343123.
Article23. Masiero S, Pierobon R, Previato C, Gomiero E. Pneumonia in stroke patients with oropharyngeal dysphagia: a six-month follow-up study. Neurol Sci. 2008; 29:139–145. PMID: 18612760.
Article24. Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992; 103:823–829. PMID: 1499933.
Article25. Logemann JA, Pauloski BR, Rademaker AW, Kahrilas PJ. Oropharyngeal swallow in younger and older women: videofluoroscopic analysis. J Speech Lang Hear Res. 2002; 45:434–445. PMID: 12068997.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Relationship between Generalized Sarcopenia and the Severity of Dysphagia after a Stroke
- Deep Learning Analysis to Automatically Detect the Presence of Penetration or Aspiration in Videofluoroscopic Swallowing Study
- Quantitative Evaluation of Dysphagia Using Scintigraphy
- Dysphagia Aortica Initially Misdiagnosed as Poststroke Dysphagia: A Case Report