Obstet Gynecol Sci.
2016 Jan;59(1):62-65. 10.5468/ogs.2016.59.1.62.
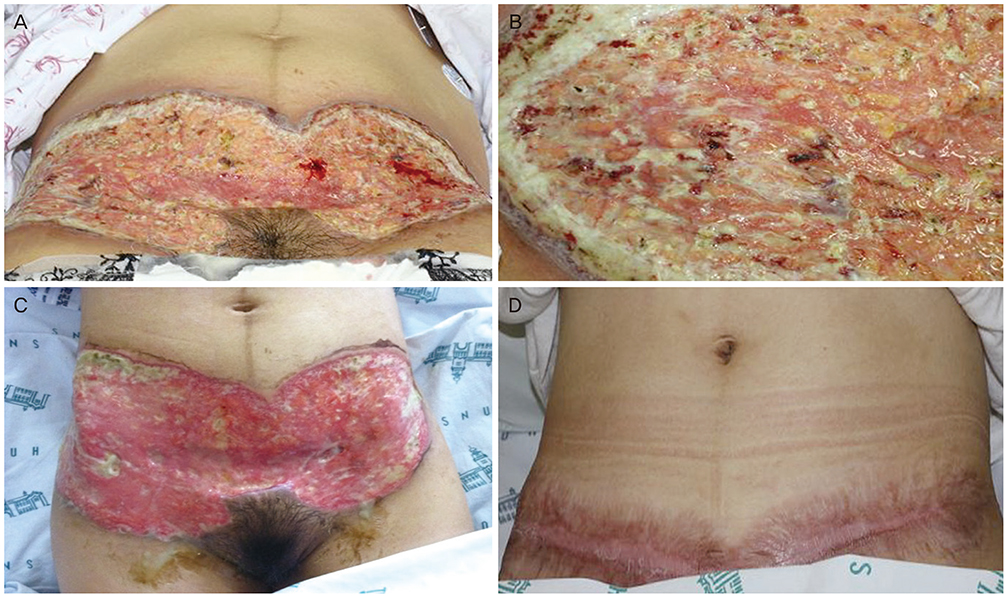
Successful vaginal birth after prior cesarean section in a patient with pyoderma gangrenosum
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea. jhs0927@snu.ac.kr
- KMID: 2152647
- DOI: http://doi.org/10.5468/ogs.2016.59.1.62
Abstract
- Pyoderma gangrenosum is an extremely rare chronic cutaneous disease causing severe ulceration. It can be developed after minor trauma or surgical procedure. The typical features mimic acute infection site, however the treatment methods are opposing since pyoderma gangrenosum is improved with the use of corticosteroids, not antibiotic therapy. We here report a patient who had been diagnosed for acute infection after cesarean delivery in 2011 and treated with a number of antibiotics, but failed to recover. The patient had suffered from pain of the disease and also renal failure caused by antibiotics. Ultimately she had been diagnosed as pyoderma gangrenosum and managed successfully with steroids. For her next pregnancy in 2013, we tried vaginal delivery after prior cesarean section and it was uneventful during and after delivery.
MeSH Terms
Figure
Reference
-
1. Amin SV, Bajapai N, Pai A, Bharatnur S, Hebbar S. Pyoderma gangrenosum in two successive pregnancies complicating caesarean wound. Case Rep Obstet Gynecol. 2014; 2014:654843.2. Ruocco E, Sangiuliano S, Gravina AG, Miranda A, Nicoletti G. Pyoderma gangrenosum: an updated review. J Eur Acad Dermatol Venereol. 2009; 23:1008–1017.3. Clark HH, Cohen PR. Pyoderma gangrenosum in an HIV-infected patient. J Am Acad Dermatol. 1995; 32(5 Pt 2):912–914.4. Callen JP, Jackson JM. Pyoderma gangrenosum: an update. Rheum Dis Clin North Am. 2007; 33:787–802.5. Reichrath J, Bens G, Bonowitz A, Tilgen W. Treatment recommendations for pyoderma gangrenosum: an evidence-based review of the literature based on more than 350 patients. J Am Acad Dermatol. 2005; 53:273–283.6. Bhat RM. Management of pyoderma gangrenosum: an update. Indian J Dermatol Venereol Leprol. 2004; 70:329–335.7. Poucke SV, Jorens PG, Peeters R, Jacobs W, de Beeck BO, Lambert J, et al. Pyoderma gangrenosum: a challenging complication of bilateral mastopexy. Int Wound J. 2004; 1:207–213.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Behcet's Disease Associated with Pyoderma Gangrenosum
- A Case of Pyoderma Gangrenosum Occurring in Behcet's Disease
- A Case of Pyoderma Gangrenosum Treated with Topical Tacrolimus and Oral Cyclosporin
- Vaginal Birth after Cesarean Delivery : Development of a Scoring System for Predicting Success Rate
- A Case of Pyoderma Gangrenosum Associated with Acute Leukemia