J Korean Soc Radiol.
2016 Jan;74(1):1-7. 10.3348/jksr.2016.74.1.1.
Balloon Dilatation Biopsy of the Biliary Stricture through the Percutaneous Transhepatic Biliary Drainage Tract: Feasibility and Diagnostic Accuracy
- Affiliations
-
- 1Department of Radiology, Kyungpook National University Hospital, Daegu, Korea. hkryeom@knu.ac.kr
- 2Public Health Medical Service, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 2150456
- DOI: http://doi.org/10.3348/jksr.2016.74.1.1
Abstract
- PURPOSE
To evaluate the feasibility and diagnostic accuracy of the balloon dilatation biopsy for the biliary stricture through the percutaneous transhepatic biliary drainage (PTBD) tract.
MATERIALS AND METHODS
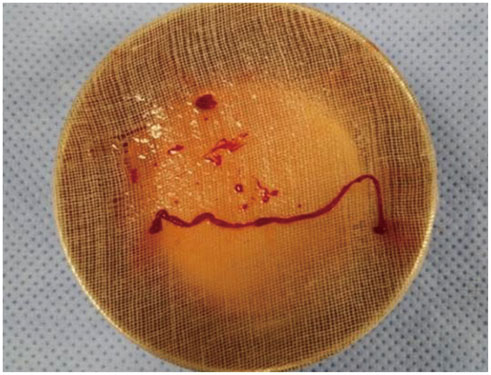
The study included 35 patients who underwent balloon dilatation biopsy for the biliary stricture through the PTBD tract. Balloon dilatation was done with a balloon catheter of 10-mm or 12-mm diameter. Soft tissue adherent to the retrieved balloon catheter and soft tissue components separated by gauze filtration of evacuated bile were sampled for histopathologic examination. The results were compared with the final diagnosis which was made by clinical and imaging follow-up for mean 989 days (n = 34) and surgery with histopathologic examination (n = 1). Procedure-related complications and diagnostic accuracy were assessed.
RESULTS
Tissues suitable for histopathologic examination were obtained in 31 out of 35 patients (88.6%). In 3 patients, self-limiting hemobilia was noted. No major complication was noted. The sensitivity, specificity, diagnostic accuracy, positive and negative predictive values for diagnosis of malignant stricture were 70.0%, 100%, 90.3%, 100%, and 87.5%, respectively.
CONCLUSION
Balloon dilatation biopsy of the biliary stricture through the PTBD tract is a feasible and accurate diagnostic method. It can be a safe alternative to the endoscopic retrograde cholangiography biopsy or forceps biopsy through the PTBD tract.
MeSH Terms
Figure
Reference
-
1. Han JK, Choi BI, Kim AY, An SK, Lee JW, Kim TK, et al. Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings. Radiographics. 2002; 22:173–187.2. Robledo R, Muro A, Prieto ML. Extrahepatic bile duct carcinoma: US characteristics and accuracy in demonstration of tumors. Radiology. 1996; 198:869–873.3. Lee WJ, Lim HK, Jang KM, Kim SH, Lee SJ, Lim JH. Radiologic spectrum of cholangiocarcinoma: emphasis on unusual manifestations and differential diagnoses. Radiographics. 2001; 21 Spec No:S97–S116.4. Welch TJ, Sheedy PF 2nd, Johnson CD, Johnson CM, Stephens DH. CT-guided biopsy: prospective analysis of 1,000 procedures. Radiology. 1989; 171:493–496.5. Droese M, Altmannsberger M, Kehl A, Lankisch PG, Weiss R, Weber K, et al. Ultrasound-guided percutaneous fine needle aspiration biopsy of abdominal and retroperitoneal masses. Accuracy of cytology in the diagnosis of malignancy, cytologic tumor typing and use of antibodies to intermediate filaments in selected cases. Acta Cytol. 1984; 28:368–384.6. Hall-Craggs MA, Lees WR. Fine-needle aspiration biopsy: pancreatic and biliary tumors. AJR Am J Roentgenol. 1986; 147:399–403.7. Kim CS, Han YM, Song HY, Choi KC, Kim DG, Cho BH. Percutaneous transhepatic biliary biopsy using gastrofiberscopic biopsy forceps. J Korean Med Sci. 1992; 7:325–332.8. Tsai CC, Mo LR, Chou CY, Han SJ, Lin RC, Kuo JY, et al. Percutaneous transhepatic transluminal forceps biopsy in obstructive jaundice. Hepatogastroenterology. 1997; 44:770–773.9. Donald JJ, Fache JS, Burhenne HJ. Percutaneous transluminal biopsy of the biliary tract. Can Assoc Radiol J. 1993; 44:185–188.10. Tapping CR, Byass OR, Cast JE. Cytological sampling versus forceps biopsy during percutaneous transhepatic biliary drainage and analysis of factors predicting success. Cardiovasc Intervent Radiol. 2012; 35:883–889.11. Cantwell CP, Pena CS, Gervais DA, Hahn PF, Dawson SL, Mueller PR. Thirty years' experience with balloon dilation of benign postoperative biliary strictures: long-term outcomes. Radiology. 2008; 249:1050–1057.12. Baron RL, Stanley RJ, Lee JK, Koehler RE, Melson GL, Balfe DM, et al. A prospective comparison of the evaluation of biliary obstruction using computed tomography and ultrasonography. Radiology. 1982; 145:91–98.13. Ryan ME. Cytologic brushings of ductal lesions during ERCP. Gastrointest Endosc. 1991; 37:139–142.14. Mendez G Jr, Russell E, Levi JU, Koolpe H, Cohen M. Percutaneous brush biopsy and internal drainage of biliary tree through endoprosthesis. AJR Am J Roentgenol. 1980; 134:653–659.15. Cropper LD Jr, Gold RE. Simplified brush biopsy of the bile ducts. Radiology. 1983; 148:307–308.16. Jung GS, Huh JD, Lee SU, Han BH, Chang HK, Cho YD. Bile duct: analysis of percutaneous transluminal forceps biopsy in 130 patients suspected of having malignant biliary obstruction. Radiology. 2002; 224:725–730.17. Patel P, Rangarajan B, Mangat K. Improved accuracy of percutaneous biopsy using "cross and push" technique for patients suspected with malignant biliary strictures. Cardiovasc Intervent Radiol. 2015; 38:1005–1010.18. Pugliese V, Conio M, Nicolò G, Saccomanno S, Gatteschi B. Endoscopic retrograde forceps biopsy and brush cytology of biliary strictures: a prospective study. Gastrointest Endosc. 1995; 42:520–526.19. Ikeda M, Maetani I, Terada K, Ukita T, Tada T, Shigoka H, et al. Usefulness of endoscopic retrograde biliary biopsy using large-capacity forceps for extrahepatic biliary strictures: a prospective randomized study. Endoscopy. 2010; 42:837–841.20. Nimura Y. Staging of biliary carcinoma: cholangiography and cholangioscopy. Endoscopy. 1993; 25:76–80.21. Savader SJ, Prescott CA, Lund GB, Osterman FA. Intraductal biliary biopsy: comparison of three techniques. J Vasc Interv Radiol. 1996; 7:743–750.22. Molnar W, Stockum AE. Transhepatic dilatation of choledochoenterostomy strictures. Radiology. 1978; 129:59–64.23. Stewart CJ, Mills PR, Carter R, O'Donohue J, Fullarton G, Imrie CW, et al. Brush cytology in the assessment of pancreatico-biliary strictures: a review of 406 cases. J Clin Pathol. 2001; 54:449–455.24. Ryan ME, Baldauf MC. Comparison of flow cytometry for DNA content and brush cytology for detection of malignancy in pancreaticobiliary strictures. Gastrointest Endosc. 1994; 40(2 Pt 1):133–139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Transhepatic Biliary Drainage and Percutaneous Balloon Dilatation for Patients with Biliary Duct Stones and Biliary Obstruction in Whom an Endoscopic Approach Is Difficult to Use: Case Series of 21 Patients at a Single Institution
- De novo hepatico-gastric stent placement for biliary stricture via percutaneous transhepatic biliary approach
- The Experience of the Percutaneous Balloon Dilatation in the Treatment of Ureteral Stricture
- Percutaneous dilatation of biliary benign strictures
- The Evaluation and Treatment of the Obstructive Biliary Disease through the Percutaneous Transhepatic Choledocoscopy (PTCS )