Korean J Pain.
2015 Jul;28(3):210-216. 10.3344/kjp.2015.28.3.210.
Infusion Methods for Continuous Interscalene Brachial Plexus Block for Postoperative Pain Control after Arthroscopic Rotator Cuff Repair
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea. shinsw@pusan.ac.kr
- 2Department of Anesthesia and Pain Medicine, Pusan National University Dental Hospital, Yangsan, Korea.
- 3Department of Anesthesia and Pain Medicine, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2149466
- DOI: http://doi.org/10.3344/kjp.2015.28.3.210
Abstract
- BACKGROUND
Infusion methods during regional analgesia using perineural catheters may influence the quality of postoperative analgesia. This study was conducted to compare the effects of combined or bolus-only infusion of 0.2% ropivacaine on the postoperative analgesia in interscalene brachial plexus block (ISBPB) with perineural catheterization.
METHODS
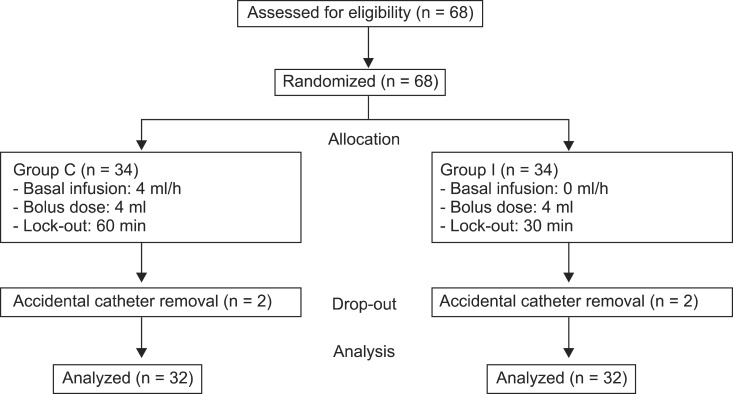
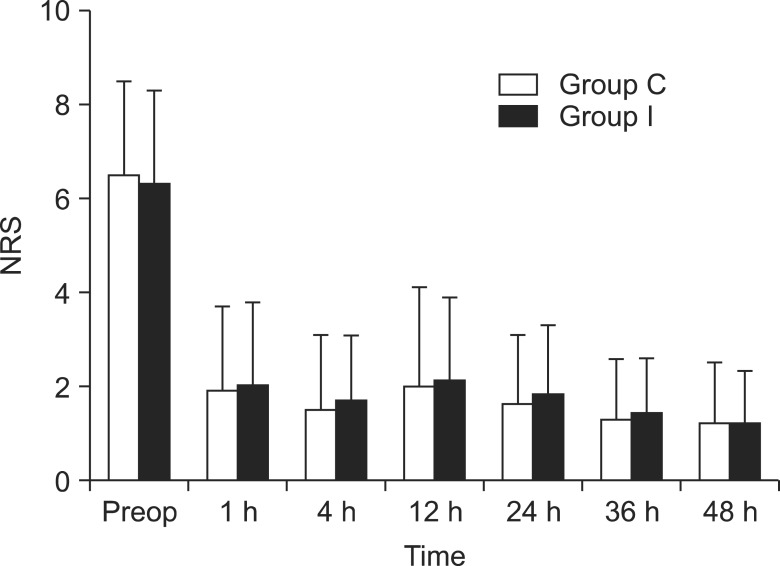
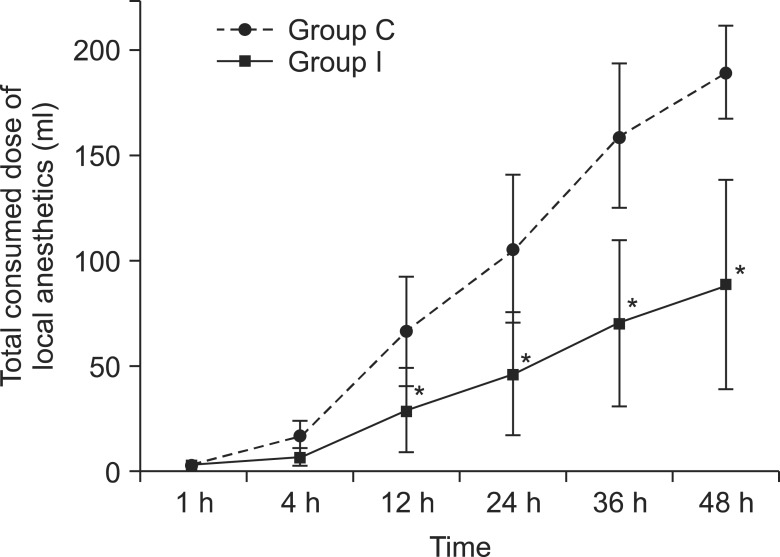
Patients scheduled for arthroscopic rotator cuff repair were divided into two groups, one that would receive a combined infusion (group C, n = 32), and one that would receive intermittent infusion (group I, n = 32). A perineural catheter was inserted into the interscalene brachial plexus (ISBP) using ultrasound (US) and nerve stimulation, and 10 ml of 0.2% ropivacaine was administered. After the operation, group C received a continuous infusion of 4 ml/h, and a 4 ml bolus with a lockout interval of 60 min. Group I received only a 4 ml bolus, and the lockout interval was 30 min. Postoperative pain by the numeric rating scale (NRS) and the forearm muscle tone by the manual muscle test (MMT) were checked and evaluated at the following timepoints: preoperative, and postoperative 1, 4, 12, 24, 36, and 48 h. Supplemental opioid requirements, total consumed dose of local anesthetic, and adverse effects were compared between the two groups.
RESULTS
Sixty-four patients completed the study and the postoperative values such as operation time, time to discharge, and operation site were comparable. There were no differences in NRS scores and supplemental opioid requirements between the two groups. The MMT scores of group I at 4 and 12 h after surgery were significantly higher than those of group C (P < 0.05). The total consumed dose of local anesthetic was significantly lower in group I than in group C (P < 0.05). The adverse effects were not different between the groups.
CONCLUSIONS
The bolus-only administration of 0.2% ropivacaine provided a similar analgesic effect with a lower total volume of local anesthetic and decreased motor weakness compared to combined infusion. Therefore, bolus-only administration is an effective postoperative analgesic method in ISBPB with perineural catheterization after rotator cuff repair.
MeSH Terms
Figure
Reference
-
1. Shin SW, Byeon GJ, Yoon JU, Ok YM, Baek SH, Kim KH, et al. Effective analgesia with ultrasound-guided interscalene brachial plexus block for postoperative pain control after arthroscopic rotator cuff repair. J Anesth. 2014; 28:64–69. PMID: 23903900.
Article2. Borgeat A, Kalberer F, Jacob H, Ruetsch YA, Gerber C. Patient-controlled interscalene analgesia with ropivacaine 0.2% versus bupivacaine 0.15% after major open shoulder surgery: the effects on hand motor function. Anesth Analg. 2001; 92:218–223. PMID: 11133631.
Article3. Ilfeld BM, Morey TE, Enneking FK. Infraclavicular perineural local anesthetic infusion: a comparison of three dosing regimens for postoperative analgesia. Anesthesiology. 2004; 100:395–402. PMID: 14739817.4. Pere P, Watanabe H, Pitkänen M, Wahlström T, Rosenberg PH. Local myotoxicity of bupivacaine in rabbits after continuous supraclavicular brachial plexus block. Reg Anesth. 1993; 18:304–307. PMID: 8268120.5. Dhir S, Ganapathy S, Lindsay P, Athwal GS. Case report: ropivacaine neurotoxicity at clinical doses in interscalene brachial plexus block. Can J Anaesth. 2007; 54:912–916. PMID: 17975237.
Article6. Shakespeare TJ, Tsui BC. Intermittent hoarseness with continuous interscalene brachial plexus catheter infusion due to deficient carotid sheath. Acta Anaesthesiol Scand. 2013; 57:1085–1086. PMID: 23808964.
Article7. Yang CW, Jung SM, Kwon HU, Cho CK, Yi JW, Kim CW, et al. A clinical comparison of continuous interscalene brachial plexus block with different basal infusion rates of 0.2% ropivacaine for shoulder surgery. Korean J Anesthesiol. 2010; 59:27–33. PMID: 20651995.
Article8. Norberg FB, Field LD, Savoie FH 3rd. Repair of the rotator cuff. Mini-open and arthroscopic repairs. Clin Sports Med. 2000; 19:77–99. PMID: 10652666.9. Kim SH, Ha KI, Park JH, Kang JS, Oh SK, Oh I. Arthroscopic versus mini-open salvage repair of the rotator cuff tear: outcome analysis at 2 to 6 years' follow-up. Arthroscopy. 2003; 19:746–754. PMID: 12966383.
Article10. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006; 367:1618–1625. PMID: 16698416.
Article11. Ilfeld BM, Morey TE, Wright TW, Chidgey LK, Enneking FK. Continuous interscalene brachial plexus block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesth Analg. 2003; 96:1089–1095. PMID: 12651666.
Article12. Park SK, Choi YS, Choi SW, Song SW. A comparison of three methods for postoperative pain control in patients undergoing arthroscopic shoulder surgery. Korean J Pain. 2015; 28:45–51. PMID: 25589946.
Article13. Egol KA, Forman J, Ong C, Rosenberg A, Karia R, Zuckerman JD. Regional anesthesia improves outcome in patients undergoing proximal humerus fracture repair. Bull Hosp Jt Dis (2013). 2014; 72:231–236. PMID: 25429392.14. Ilfeld BM, Moeller LK, Mariano ER, Loland VJ, Stevens-Lapsley JE, Fleisher AS, et al. Continuous peripheral nerve blocks: is local anesthetic dose the only factor, or do concentration and volume influence infusion effects as well? Anesthesiology. 2010; 112:347–354. PMID: 20098137.15. Fredrickson MJ, Ball CM, Dalgleish AJ. Posterior versus anterolateral approach interscalene catheter placement: a prospective randomized trial. Reg Anesth Pain Med. 2011; 36:125–133. PMID: 21425511.
Article16. Hogan Q, Dotson R, Erickson S, Kettler R, Hogan K. Local anesthetic myotoxicity: a case and review. Anesthesiology. 1994; 80:942–947. PMID: 8024149.
Article17. Zink W, Bohl JR, Hacke N, Sinner B, Martin E, Graf BM. The long term myotoxic effects of bupivacaine and ropivacaine after continuous peripheral nerve blocks. Anesth Analg. 2005; 101:548–554. PMID: 16037174.
Article18. Avellanet M, Sala-Blanch X, Rodrigo L, Gonzalez-Viejo MA. Permanent upper trunk plexopathy after interscalene brachial plexus block. J Clin Monit Comput. 2015; [in press].
Article19. Jenkins CR, Karmakar MK. An unusual complication of interscalene brachial plexus catheterization: delayed catheter migration. Br J Anaesth. 2005; 95:535–537. PMID: 16051648.
Article20. Singelyn FJ, Seguy S, Gouverneur JM. Interscalene brachial plexus analgesia after open shoulder surgery: continuous versus patient-controlled infusion. Anesth Analg. 1999; 89:1216–1220. PMID: 10553837.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Regional nerve blocks for relieving postoperative pain in arthroscopic rotator cuff repair
- Effectiveness of Multimodal Pain Control in Early Phase After Arthroscopic Rotator Cuff Repair
- Comparison of Analgesic Efficacy between Single Interscalene Block Combined with a Continuous Intra-bursal Infusion of Ropivacaine and Continuous Interscalene Block after Arthroscopic Rotator Cuff Repair
- A clinical comparison of continuous interscalene brachial plexus block with different basal infusion rates of 0.2% ropivacaine for shoulder surgery
- Hypoesthesia of the Cutaneous Branch of Cervical Plexus after Shoulder Arthroscopy under General Anesthesia with Ultrasound Guided-Interscalene Block