Korean Circ J.
2010 Aug;40(8):377-386. 10.4070/kcj.2010.40.8.377.
Prognostic Value of Initial Echocardiographic Features in Patients With Tuberculous Pericarditis
- Affiliations
-
- 1Division of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jmsong@amc.seoul.kr
- 2Division of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2145529
- DOI: http://doi.org/10.4070/kcj.2010.40.8.377
Abstract
- BACKGROUND AND OBJECTIVES
Tuberculous (TB) pericarditis is a major cause of constrictive pericarditis requiring pericardiectomy. We sought to determine initial prognostic factors in patients with TB pericarditis.
SUBJECTS AND METHODS
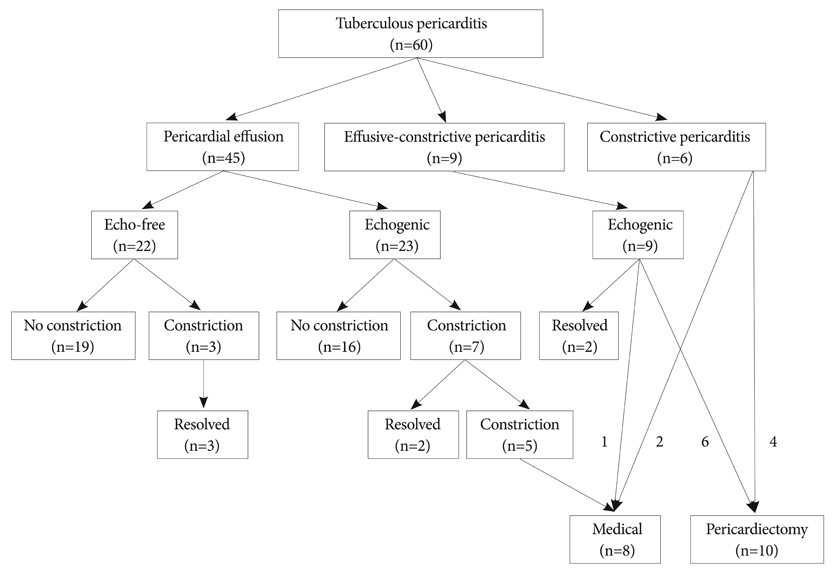
We evaluated initial presentation and clinical outcomes (mean follow-up 32+/-27 months) in 60 consecutive patients newly diagnosed with TB pericarditis.
RESULTS
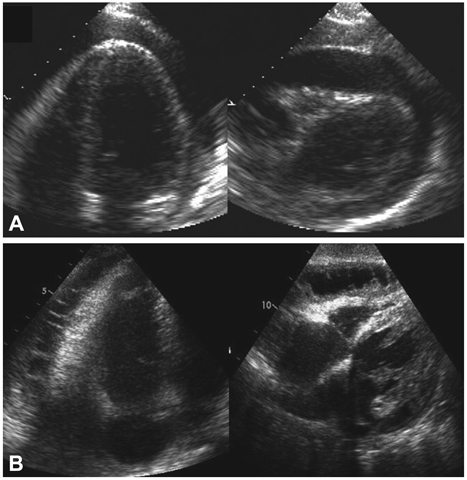
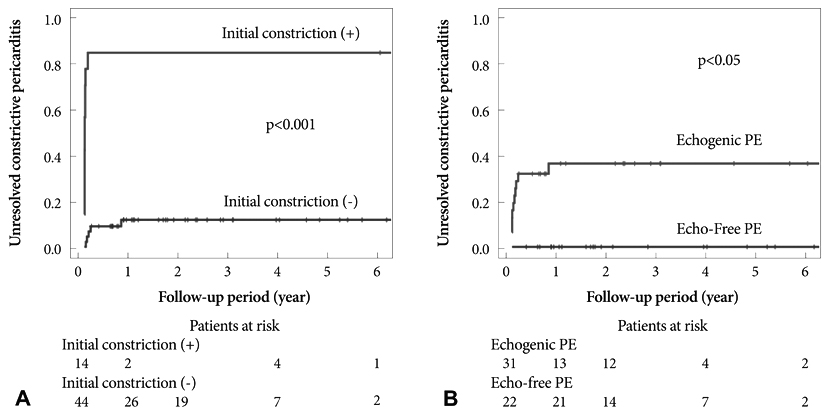
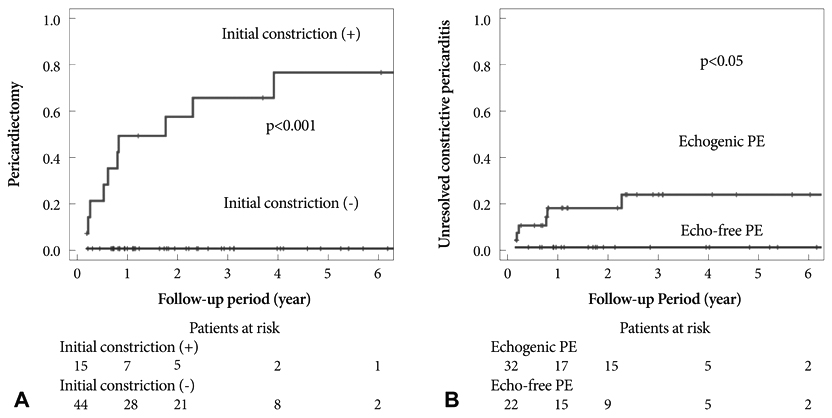
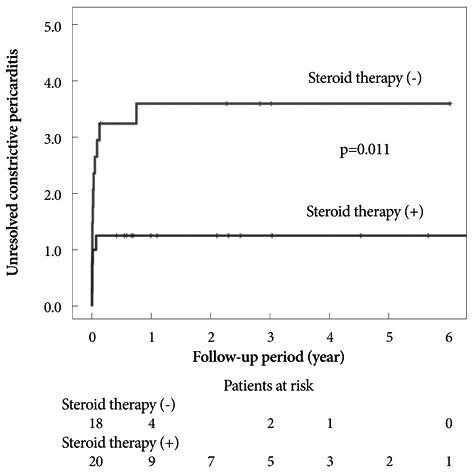
Initial presentations were pericardial effusion (PE), effusive-constrictive pericarditis, and constrictive pericarditis in 45 (75%), 9 (15%), and 6 (10%) patients, respectively. Of the 54 patients without initial constrictive pericarditis, 32 (59%) showed echogenic materials in PE, including frond-like exudative coating and fibrinous strands. These patients had a longer disease duration before diagnosis, were initially more symptomatic, in a more advanced state, showed more persistent pericardial constrictions (38% vs. 0%, p<0.001) despite anti-TB medications, and tended to require pericardiectomy more often (19% vs. 0%, p=0.07, p<0.05 by Kaplan-Meier). All patients with effusive-constrictive pericarditis showed echogenic PE. Of the 60 total patients, 10 (17%) underwent pericardiectomies during follow-up. All of these patients showed initial pericardial constrictions, whereas no patient without initial pericardial constriction underwent pericardiectomy (p<0.001). Seven patients showed transient pericardial constrictions that resolved without pericardiectomy.
CONCLUSION
Initial pericardial constriction and echogenic PE are poor prognostic signs for persistent pericardial constriction and pericardiectomy in patients with newly diagnosed TB pericarditis. These results suggest that early diagnosis and prompt anti-TB medication may be critical.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Early Testing and Prompt Initiation of Proper Treatment: a Clever Strategy to Fight with Tuberculosis Pericarditis
Iksung Cho, William Dowon Kim
Korean Circ J. 2020;50(7):610-612. doi: 10.4070/kcj.2020.0179.
Reference
-
1. Zumla A, Mwaba P, Huggett J, Kapata N, Chanda D, Grange J. Reflections on the white plague. Lancet Infect Dis. 2009. 9:197–202.2. Mayosi BM, Wiysonge CS, Ntsekhe M, et al. Clinical characteristics and initial management of patients with tuberculous pericarditis in the HIV era: the Investigation of the Management of Pericarditis in Africa (IMPI Africa) registry. BMC Infect Dis. 2006. 6:2.3. Syed FF, Mayosi BM. A modern approach to tuberculous pericarditis. Prog Cardiovasc Dis. 2007. 50:218–236.4. Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation. 2005. 112:3608–3616.5. Mayosi BM, Volmink JA, Commerford PJ. Pericardial Disease: an Evidence-Based Approach to Diagnosis and Treatment. 2003. 2nd ed. London: BMJ Books.6. Suwan PK, Potjalongsilp S. Predictors of constrictive pericarditis after tuberculous pericarditis. Br Heart J. 1995. 73:187–189.7. Hageman JH, D Esopo ND, Glenn WW. Tuberculosis of the pericardium: a long-term analysis of forty-four proved cases. N Engl J Med. 1964. 270:327–332.8. Williams IP, Hetzel MR. Tuberculous pericarditis in south-west London: an increasing problem. Thorax. 1978. 33:816–817.9. Komsuoglu B, Goldeli O, Kulan K, Gedik Y. Tuberculous pericarditis in north-east Turkey: an echocardiographic study. Acta Cardiol. 1994. 49:157–163.10. Long R, Younes M, Patton N, Hershfield E. Tuberculous pericarditis: long-term outcome in patients who received medical therapy alone. Am Heart J. 1989. 117:1133–1139.11. Ng TT, Strang JI, Wilkins EG. Serodiagnosis of pericardial tuberculosis. QJM. 1995. 88:317–320.12. Komsuoglu B, Goldeli O, Kulan K, Komsuoglu SS. The diagnostic and prognostic value of adenosine deaminase in tuberculous pericarditis. Eur Heart J. 1995. 16:1126–1130.13. Kim SH, Song JM, Jung IH, Kim MJ, Kang DH, Song JK. Initial echocardiographic characteristics of pericardial effusion determine the pericardial complications. Int J Cardiol. 2009. 136:151–155.14. Chia BL, Choo M, Tan A, Ee B. Echocardiographic abnormalities in tuberculous pericardial effusion. Am Heart J. 1984. 107:1034–1035.15. George S, Salama AL, Uthaman B, Cherian G. Echocardiography in differentiating tuberculous from chronic idiopathic pericardial effusion. Heart. 2004. 90:1338–1339.16. Ku CS, Chiou KR, Lin SL, Liu CP, Chaing HT. Echocardiographic features of tuberculous pericarditis. J Chin Med Assoc. 2003. 66:613–616.17. Liu PY, Li YH, Tsai WC, et al. Usefulness of echocardiographic intrapericardial abnormalities in the diagnosis of tuberculous pericardial effusion. Am J Cardiol. 2001. 87:1133–1135.18. Yang CC, Lee MH, Liu JW, Leu HS. Diagnosis of tuberculous pericarditis and treatment without corticosteroids at a tertiary teaching hospital in Taiwan: a 14-year experience. J Microbiol Immunol Infect. 2005. 38:47–52.19. Park SY. The usefulness of pericardial biopsy to evaluate the causes of pericardial disease. Korean Circ J. 1999. 29:517–522.20. Hinds SW, Reisner SA, Amico AF, Meltzer RS. Diagnosis of pericardial abnormalities by 2D-echo: a pathology-echocardiography correlation in 85 patients. Am Heart J. 1992. 123:143–150.21. Oh JK, Hatle LK, Seward JB, et al. Diagnostic role of Doppler echocardiography in constrictive pericarditis. J Am Coll Cardiol. 1994. 23:154–162.22. Jung HG. Respiratory variations of Doppler echocardiographic parameters in cardiac tamponade. Korean Circ J. 1998. 28:412–424.23. Dal-Bianco JP, Sengupta PP, Mookadam F, Chandrasekaran K, Tajik AJ, Khandheria BK. Role of echocardiography in the diagnosis of constrictive pericarditis. J Am Soc Echocardiogr. 2009. 22:24–33.24. Come PC, Miklozek CL, Riley MF, Carl LV, Morgan JP. Echocardiographic changes in rapidly developing pericardial constriction. Am Heart J. 1985. 109:1385–1387.25. Sinha PR, Singh BP, Jaipuria N, Rao KD, Shetty GG, Avasthey P. Intrapericardial echogenic images and development of constrictive pericarditis in patients with pericardial effusion. Am Heart J. 1996. 132:1268–1272.26. Haley JH, Tajik AJ, Danielson GK, Schaff HV, Mulvagh SL, Oh JK. Transient constrictive pericarditis: causes and natural history. J Am Coll Cardiol. 2004. 43:271–275.27. Yang HS, Song JK, Song JM, et al. Clinical characteristics of constrictive pericarditis diagnosed by echo-Doppler technique in Korea. J Korean Med Sci. 2001. 16:558–566.28. Oh JK, Tajik AJ, Appleton CP, Hatle LK, Nishimura RA, Seward JB. Preload reduction to unmask the characteristic Doppler features of constrictive pericarditis: a new observation. Circulation. 1997. 95:796–799.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Course of Tuberculous Pericarditis in Immunocompetent Hosts Based on Serial Echocardiography
- Tuberculous Pericarditis Mimicking a Malignant Pericardial Tumor: A Case Report
- A Case of Tuberculous Pericarditis Diagnosed by Increased ADA Activity in Pericardial Fluid
- A case of tuberculous pericarditis presenting as pericardial mass compressing pulmonary artery
- Ga-67 SPECT Finding in Tuberculous Pericarditis with Mediastinal Mass: A case report