J Cardiovasc Ultrasound.
2015 Dec;23(4):266-270. 10.4250/jcu.2015.23.4.266.
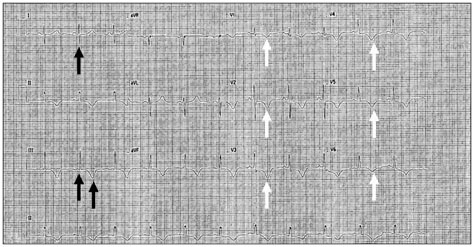
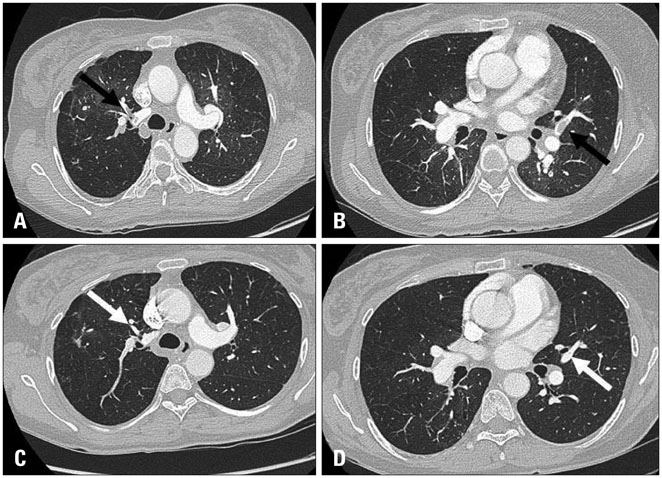
A Case of Klippel-Trenaunay Syndrome with Acute Submassive Pulmonary Thromboembolism Treated with Thrombolytic Therapy
- Affiliations
-
- 1Department of Internal Medicine, National Medical Center, Seoul, Korea. seo0515@medimail.co.kr
- 2Cardiovascular Center, National Medical Center, Seoul, Korea.
- KMID: 2144459
- DOI: http://doi.org/10.4250/jcu.2015.23.4.266
Abstract
- Klippel-Trenaunay syndrome is a rare congenital mesodermal abnormality characterized by varicose veins, cutaneous hemangiomas, soft tissue and bony hypertrophy of limb. Potential complications such as deep venous thrombosis and pulmonary thromboembolism have not been reported in Korea to date. We demonstrate the case of a 48-year-old woman with Klippel-Trenaunay syndrome with extensive varicose veins on right lower limb, hypertrophy of left big toe and basilar artery tip aneurysm, complicated with acute submassive pulmonary thromboembolism treated successfully with intravenous thrombolytic therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Huiras EE, Barnes CJ, Eichenfield LF, Pelech AN, Drolet BA. Pulmonary thromboembolism associated with Klippel-Trenaunay syndrome. Pediatrics. 2005; 116:e596–e600.2. Jacob AG, Driscoll DJ, Shaughnessy WJ, Stanson AW, Clay RP, Gloviczki P. Klippel-Trénaunay syndrome: spectrum and management. Mayo Clin Proc. 1998; 73:28–36.3. Baskerville PA, Ackroyd JS, Lea Thomas M, Browse NL. The Klippel-Trenaunay syndrome: clinical, radiological and haemodynamic features and management. Br J Surg. 1985; 72:232–236.4. Mazoyer E, Enjolras O, Laurian C, Houdart E, Drouet L. Coagulation abnormalities associated with extensive venous malformations of the limbs: differentiation from Kasabach-Merritt syndrome. Clin Lab Haematol. 2002; 24:243–251.5. Oduber CE, van Beers EJ, Bresser P, van der Horst CM, Meijers JC, Gerdes VE. Venous thromboembolism and prothrombotic parameters in Klippel-Trenaunay syndrome. Neth J Med. 2013; 71:246–252.6. Muluk SC, Ginns LC, Semigran MJ, Kaufman JA, Gertler JP. Klippel-Trénaunay syndrome with multiple pulmonary emboli--an unusual cause of progressive pulmonary dysfunction. J Vasc Surg. 1995; 21:686–690.7. Ndzengue A, Rafal RB, Balmir S, Rai DB, Jaffe EA. Klippel-Trenaunay syndrome: an often overlooked risk factor for venous thromboembolic disease. Int J Angiol. 2012; 21:233–236.8. Yamada T, Ohba T, Yamamoto T, Kimata N, Inami T, Munakata R, Murakami D, Maruyama M, Takano M, Ibuki C, Hata N, Seino Y, Mizuno K. A 17-year-old girl with Klippel-Weber syndrome complicated with a pulmonary thromboembolism and RV thrombus. Intern Med. 2013; 52:1337–1340.9. Star A, Fuller CE, Landas SK. Intracranial aneurysms in Klippel-Trenaunay/Weber syndromes: case report. Neurosurgery. 2010; 66:E1027–E1028. discussion E102810. Kim HJ, Kim SC. A case of pseudo-Kaposi's sarcoma associated with Klippel-Trenaunay syndrome. Korean J Dermatol. 2006; 44:450–453.11. Lee YK, Kim JK, Cho KS. Bladder hemangioma associated with Klippel-Trenaunay syndrome: case report. J Korean Radiol Soc. 2003; 48:271–274.12. Chung YW, Han DS, Paik CH, Park YK, Kim JP, Lee HL, Kim JB, Sohn JH, Hahm JS, Park HK. A case of Klippel-Trenaunay-Weber syndrome with sigmoid varices. Korean J Gastrointest Endosc. 2003; 27:21–25.13. Kim JY, Lee JB, Lee SC, Won YH. A case of Klippel-Trenaunay syndrome with lymphangioma circumscriptum. Korean J Dermatol. 2000; 38:1522–1526.14. Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P, Vedantham S, White RJ, Zierler BK. American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. American Heart Association Council on Peripheral Vascular Disease. American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011; 123:1788–1830.15. Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, Vonk Noordegraaf A, Zamorano JL, Zompatori M. Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014; 35:3033–3069. 3033a–3069k.16. Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, Bluhmki E, Bouvaist H, Brenner B, Couturaud F, Dellas C, Empen K, Franca A, Galiè N, Geibel A, Goldhaber SZ, Jimenez D, Kozak M, Kupatt C, Kucher N, Lang IM, Lankeit M, Meneveau N, Pacouret G, Palazzini M, Petris A, Pruszczyk P, Rugolotto M, Salvi A, Schellong S, Sebbane M, Sobkowicz B, Stefanovic BS, Thiele H, Torbicki A, Verschuren F, Konstantinides SV. PEITHO Investigators. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med. 2014; 370:1402–1411.17. Sumner CJ, Golden JA, Hemphill JC 3rd. Should thrombolysis be contraindicated in patients with cerebral arteriovenous malformations. Crit Care Med. 2002; 30:2359–2362.18. Edwards NJ, Kamel H, Josephson SA. The safety of intravenous thrombolysis for ischemic stroke in patients with pre-existing cerebral aneurysms: a case series and review of the literature. Stroke. 2012; 43:412–416.