Korean J Endocr Surg.
2015 Mar;15(1):15-19. 10.16956/kaes.2015.15.1.15.
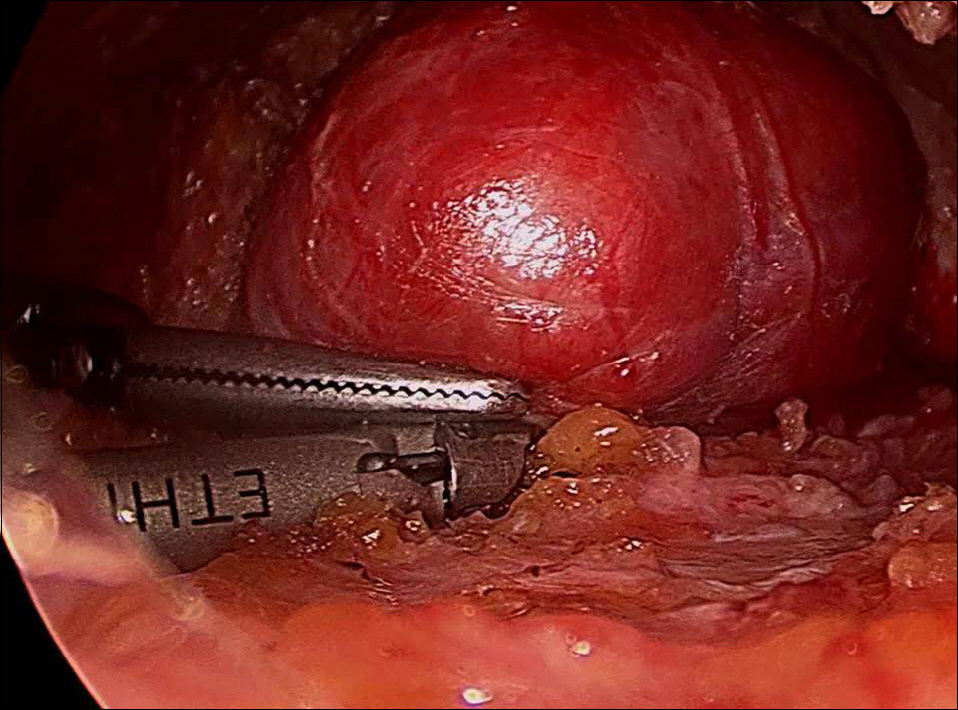
Cystic Medullary Thyroid Carcinoma: A Case of Undergoing Endoscopic Thyroid Lobectomy
- Affiliations
-
- 1Department of Pathology, Gachon University Gil Medical Center, Incheon, Korea.
- 2Department of Surgery, Gachon University Gil Medical Center, Incheon, Korea. dryooseung@gilhospital.com
- KMID: 2144009
- DOI: http://doi.org/10.16956/kaes.2015.15.1.15
Abstract
- On ultrasonography, medullary thyroid carcinoma (MTC) shows hypoechogenicity, an irregular margin, a predominantly solid composition, and microcalcifications, similar to those observed in papillary thyroid carcinoma (PTC). MTC presenting as a cystic lesion is rare, and endoscopic thyroidectomy can be performed for benign thyroid masses and early stage PTC, however it is inappropriate for MTC regardless of cystic change. The authors report a case of cystic MTC found after endoscopic thyroid lobectomy and provide a review of the literature on this topic.
Figure
Reference
-
References
1. The Korea Central Cancer Registry, Ministry of Health and Welfare. National Cancer Registration and Statistics in Korea;2011.2. DeLellis RA, Lloyd RV, Heitz PU, Eng C. WHO Classification of Tumors, Pathology and genetics of tumors of endocrine organs. Lyon, France: IARCpress;2004.3. Nikiforov YE, Biddinger PW, Thompson LD. Diagnostic pathology and molecular genetics of the thyroid. 2nd ed.Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins;2012.4. Cusick EL, McIntosh CA, Krukowski ZH, Matheson NA. Cystic change and neoplasia in isolated thyroid swellings. Br J Surg. 1988; 75:982–3.
Article5. Hiromura T. Ultrasonography of cystic thyroid nodules: sonographic-pathologic correlation. Nihon Igaku Hoshasen Gakkai Zasshi. 1994; 54:500–9.6. Lin JD, Hsuen C, Chen JY, Liou MJ, Chao TC. Cystic change in thyroid cancer. ANZ J Surg. 2007; 77:450–4.
Article7. Lee MJ, Kim EK, Kwak JY, Kim MJ. Partially cystic thyroid nodules on ultrasound: probability of malignancy and sonographic differentiation. Thyroid. 2009; 19:341–6.
Article8. Henrichsen TL, Reading CC, Charboneau JW, Donovan DJ, Sebo TJ, Hay ID. Cystic change in thyroid carcinoma: Prevalence and estimated volume in 360 carcinomas. J Clin Ultrasound. 2010; 38:361–6.
Article9. Simcic KJ, Bowland WF. Cystic medullary thyroid cancer. Surgery. 1995; 117:356–7.
Article10. Liberatore E, Emmolo I. Cystic medullary thyroid cancer. Surgery. 1996; 120:903.
Article11. Fadda G, Muie A, Rufini V, Ardito G, Revelli L, Fiorino MC, et al. Cystic medullary thyroid carcinoma: report of a case with morphological and clinical correlations. Endocr Pathol. 2000; 11:373–7.
Article12. Ozkara SK, Gürbüz Y, Müezzinoğlu B, Yumbal Z. Encapsulated cystic papillary variant of medullary carcinoma of thyroid gland. Endocr Pathol. 2002; 13:167–71.13. Kim JY, Choi JJ, Kim AH, Moon HJ, Kim EK, Kwak JY, et al. medullary thyroid carcinoma presenting as a predominantly cystic mass on ultrasonography: a case report. J Korean Soc Ultrasound Med. 2012; 31:23–6.14. Rosai J, Carcangiu ML, DeLellis RA. Tumors of thyroid gland. Atlas of tumors pathology 3rd Series, Fascicle 5. Washington, DC: Armed Forces Institute of Pathology;1992.15. Kim SH, Kim BS, Jung SL, Lee JW, Yang PS, Kang BJ, et al. Ultrasonographic findings of medullary thyroid carcinoma: a comparison with papillary thyroid carcinoma. Korean J Radiol. 2009; 10:101–5.
Article16. Lee S, Shin JH, Han BK, Ko EY. Medullary thyroid carcinoma: comparison with papillary thyroid carcinoma and application of current sonographic criteria. AJR Am J Roentgenol. 2010; 194:1090–4.
Article17. Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, et al. Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg. 2007; 31:2302–6.
Article18. Choi JY, Lee KE, Chung KW, Kim SW, Choe JH, Koo do H, et al. Endoscopic thyroidectomy via bilateral axillobreast approach (BABA): review of 512 cases in a single institute. Surg Endosc. 2012; 26:948–55.
Article19. Kim SJ, Lee KE, Choe JH, Lee J, Koo do H, Oh SK, et al. Endoscopic completion thyroidectomy by the bilateral axillobreast approach. Surg Laparosc Endosc Percutan Tech. 2010; 20:312–6.
Article20. Yi KH, Park YJ, Koong SS, Kim JH, Na DG, Ryu JS, et al. Revised Korean thyroid association management guidelines for patients with thyroid nodules and thyroid cancer. J Korean Thyroid Assoc. 2010; 3:65–96.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Medullary Thyroid Carcinoma Presenting as a Predominantly Cystic Mass on Ultrasonography: A Case Report
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma
- Medullary and Papillary Thyroid Carcinoma as a Collision Tumor: Report of Five Cases