Korean J Urol.
2007 Feb;48(2):163-170. 10.4111/kju.2007.48.2.163.
Comparison of Pain Control Method and Assessment on Postoperative Pain in Pediatric Urological Surgery of Penoscrotal and Inguinal Regions
- Affiliations
-
- 1Department of Urology, College of Medicine, Pusan National University, Korea. lsd@pusan.ac.kr
- 2Department of Urology, College of Medicine, Kosin University, Korea.
- 3Department of Anesthesiology and Pain Medicine, College of Medicine, Pusan National University, Busan, Korea.
- KMID: 2139755
- DOI: http://doi.org/10.4111/kju.2007.48.2.163
Abstract
-
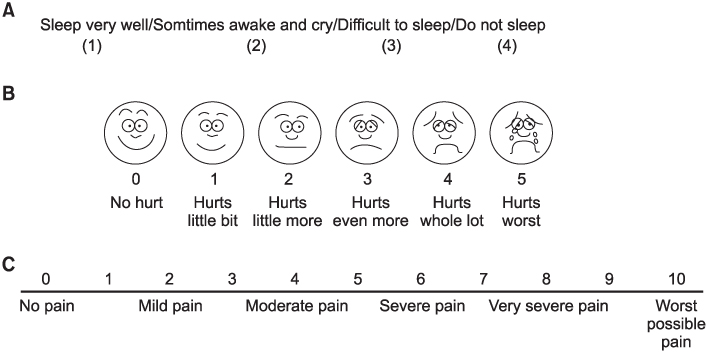
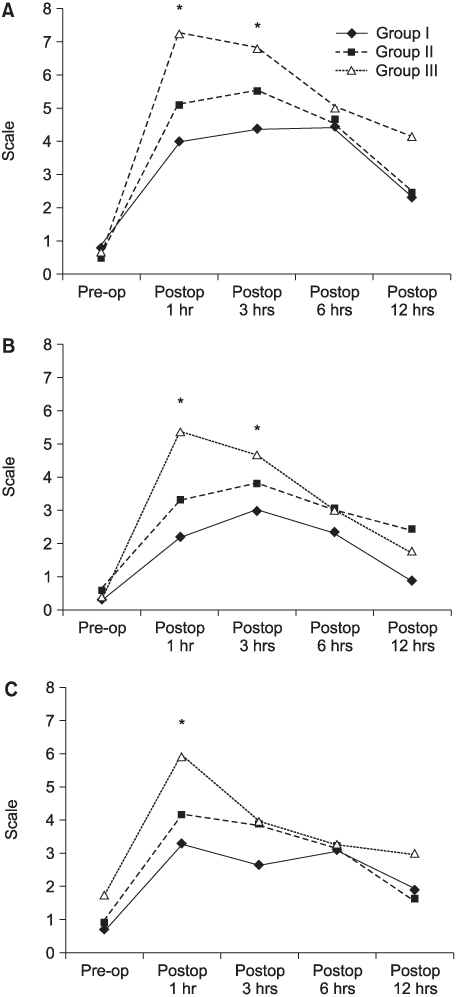
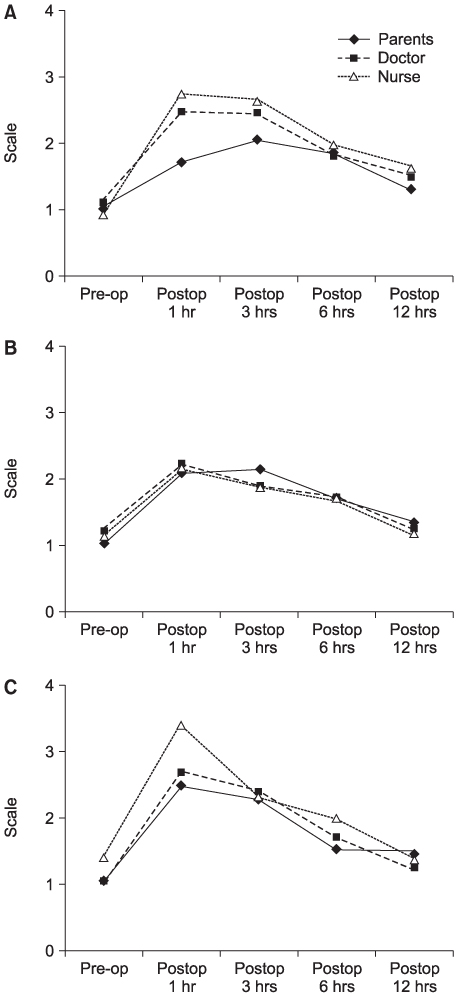
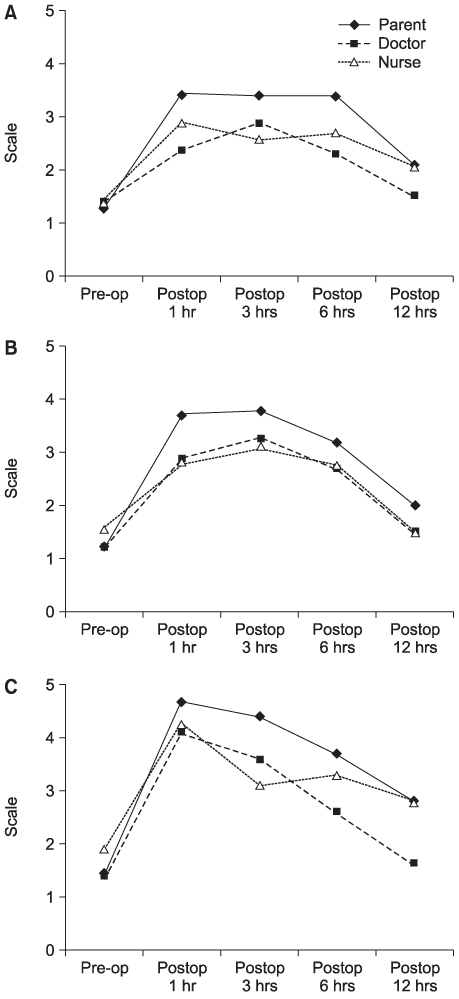
PURPOSE: This study was designed to evaluate the effects of caudal block or/and local infiltration on postoperative pain control in pediatric patients, and whether the faces pain rating scale (FPS), visual analogue scale (VAS) or sleep disturbance scale (SDS) values were estimator dependent (parents, doctors and nurses).
MATERIALS AND METHODS
Thirty four children (average age 2.8+/-2.4 years), undergoing inguinal and scrotal surgery, were randomly allocated to one of three groups; combined caudal block with local infiltration (group I), caudal block only (group II) and neither of the above two (group III). Parents, doctors and nurses assessed the FPS, VAS and SDS before and after surgery, and the side effects were assessed after surgery.
RESULTS
The mean SDS, FPS and VAS values in Group III were significantly higher than those in groups I and II at 1 and 3 hours postoperatively. All patients slept with a discontented look 1 hour postoperatively, but gradually improved and normalized 12 hours postoperatively. The mean FPS and VAS values were highest 1 hour postoperatively, and decreased with time in all groups. The mean pain value, as assessed by parents, tended to be higher than those assessed by healthcare professionals - doctors and nurses, but the correlation between the parents and healthcare professionals for the SDS, FPS and VAS assessments was statistically significant (intraclass correlation coefficients; 0.64, p<0.05). There were no side effects in any patient. CONCLISIONS: This study suggests that caudal block with local infiltration may be more useful for postoperative pain control, and all three pain scales are useful for assessing the postoperative pain associated with pediatric urological surgery of the penoscrotal and inguinal regions.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The safety of a mixture of bupivacaine and lidocaine in children after urologic inguinal and scrotal surgery
Kyoung Lee, Jae Min Chung, Sang Don Lee
Investig Clin Urol. 2018;59(2):141-147. doi: 10.4111/icu.2018.59.2.141.
Reference
-
1. Cho HS, Lee SY, Seo JO, Kim YH, Kim GS, Kim CS, et al. An experience of anesthesia for ambulatory surgery. Korean J Anesthesiol. 1997. 32:289–296.2. McGown RG. Caudal analgesia in children. Five hundred cases for procedures below the diaphragm. Anaesthesia. 1982. 37:806–818.3. Broadman LM, Hannallah RS, Norden JM. "Kiddie caudals": experience with 1,154 consecutive cases without complications. Anesth Analg. 1987. 66:S18.4. Dalens B, Hasnaoui A. Caudal anesthesia in pediatric surgery: success rate and adverse effects in 750 consecutive patients. Anesth Analg. 1989. 68:83–89.5. Payne KA, Hendrix MR, Wade WJ. Caudal bupivacaine for postoperative analgesia in pediatric lower limb surgery. J Pediatr Surg. 1993. 28:155–157.6. Lee JH, Chung CJ, Chin YJ. The effects of clonidine in pediatric caudal anesthesia. Korean J Anesthesiol. 1997. 33:104–111.7. Wilton NC. Postoperative pain management for pediatric urologic surgery. Urol Clin North Am. 1995. 22:189–203.8. Schulte SO, Rahlfs VW. Spread of extradural analgesia following caudal injection caudal injection in children. Br J Anaesth. 1977. 49:1024–1034.9. Ved SA, Pinosky M, Nicodemus H. Ventricular tachycardia and brief cardiovascular collapse in two infants after caudal anesthesia using a bupivacaine epinephrine solution. Anesthesiology. 1993. 79:1121–1123.10. Freid EB, Bailey AG, Valley RD. Electrocardiographic and hemodynamic changes associated with unintentional intravascular injection of bupivacaine with epinephrine in infants. Anesthesiology. 1993. 79:394–398.11. Krane EJ. Delayed respiratory depression in a child after caudal epidural morphine. Anesth Analg. 1989. 67:79–82.12. Knudsen K, Suurkula MB, Blomberg S, Sjovall J, Edvardsson N. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997. 78:507–514.13. Zaric D, Nydahl PA, Philipson L, Samuelsson L, Heierson A, Axelsson K. The effect of continuous lumbar epidural infusion of ropivacaine (0.1%, 0.2%, and 0.3%) and 0.25% bupivacaine on sensory and motor block in volunteers: a double-blind study. Reg Anesth. 1996. 21:14–25.14. Bosenberg A, Thomas J, Lopez T, Lybeck A, Huizar K, Larsson LE. The efficacy of caudal ropivacaine 1, 2 and 3 mg/ml x1 (-1) for postoperative analgesia in children. Paediatr Anaesth. 2002. 12:53–58.15. Bovill JG, Sebel PS, Stanley TH. Opioid analgesics in anesthesia: with special reference to their use in cardiovascular anesthesia. Anesthesiology. 1984. 61:731–755.16. Pyne K, Heydenrych JJ, Martins M, Samuels G. Caudal block for analgesia after pediatric inguinal surgery. S Afr Med J. 1987. 72:629–630.17. Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994. 56:217–226.18. Splinter WM, Bass J, Komocar L. Regional anaesthesia for hernia repair in children: local vs caudal anaesthesia. Can J Anaesth. 1995. 42:197–200.19. Fell D, Derrington MC, Taylor E, Wandless JG. Pediatric postoperative analgesia. A comparison between caudal block and wound infiltration of local anesthetic. Anaesthesia. 1988. 43:107–110.20. Lee YM, Leem JG, An HW, Yang HS, Lee DM, Chung SL. Effects of ketamine and clonidine for caudal analgesia produced by bupivacaine in pediatric ambulatory surgery. Korean J Anesthesiol. 1998. 34:585–591.21. Dalens B. Regional anesthesia in children. Anesth Analg. 1989. 68:654–672.22. Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988. 14:9–17.23. Chambers CT, Hardial J, Craig KD, Court C, Montgomery C. Faces scales for the measurement of postoperative pain intensity in children following minor surgery. Clin J Pain. 2005. 21:277–285.24. Kokinsky E, Thornberg E, Ostlund AL, Larsson LE. Postoperative comfort in paediatric outpatient surgery. Paediatr Anaesth. 1999. 9:243–251.25. Maciocia PM, Strachan EM, Akram AR, Hendrie RE, Kelly DN, Kemp A, et al. Pain assessment in the paediatric emergency department: whose view counts? Eur J Emerg Med. 2003. 10:264–267.26. Hicks CL, von Baeyer CL, Spafforda PA, van Korlaarc I, Goodenough B. The faces pain scale-revised: toward a common metric in pediatric pain measurement. Pain. 2001. 93:173–183.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Attention to postoperative pain control in children
- Effects of Intravenous Ketorolac and Wound Infiltration for Postoperative Pain after Inguinal Herniorrhaphy in Pediatric Surgery
- Comparison of single-dose nalbuphine versus tramadol for postoperative pain management in children: a randomized, controlled trial
- The Effect of Acupuncture on Relieving Pain after Inguinal Surgeries
- Intraoperative Bupivacaine Irrigation for Analgesia after Inguinoscrotal Surgery in Children