J Cardiovasc Ultrasound.
2013 Dec;21(4):165-170. 10.4250/jcu.2013.21.4.165.
Effect of Mitral Inflow Pattern on Diagnosis of Severe Mitral Regurgitation in Patients with Chronic Organic Mitral Regurgitation
- Affiliations
-
- 1Division of Cardiovascular Diseases, Mayo Clinic, Scottsdale, AZ, USA. chaliki.hari@mayo.edu
- KMID: 2135414
- DOI: http://doi.org/10.4250/jcu.2013.21.4.165
Abstract
- BACKGROUND
To determine sensitivity and specificity of E wave velocity in patients with severe chronic organic mitral regurgitation (MR) and normal left ventricular ejection fraction (EF) and to evaluate prevalence of A wave dominance in patients with severe MR.
METHODS
We compared 35 patients with quantified severe, chronic, quantified, organic MR due to flail/prolapsed leaflets who had reparative surgery with 35 age-matched control subjects. Exclusion criteria: EF < 60%, atrial fibrillation, and more than mild aortic regurgitation.
RESULTS
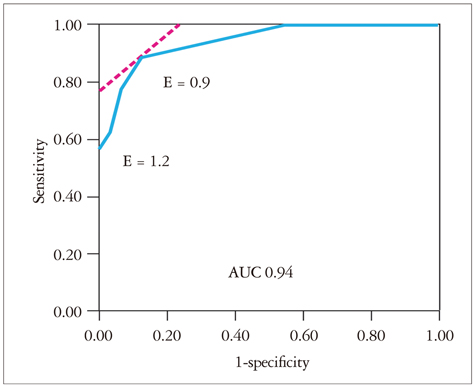
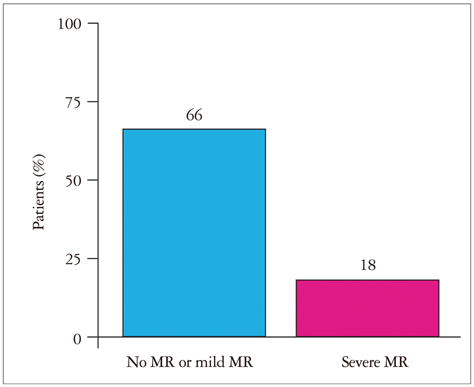
Mean [standard deviation (SD)] age [70 (8) years vs. 69 (8) years; p = 0.94] and mean (SD) EF [66% (6%) vs. 65% (4%); p = 0.43] were not different between the two groups. Mean (SD) E wave velocity was greater in case patients than control subjects [1.2 (0.3) m/sec vs. 0.7 (0.15) m/sec; p < 0.001]. However, E wave velocity of 1.2 m/sec had a sensitivity of only 57% [95% confidence interval (CI), 41-7 and a specificity of 100% (95% CI, 90-100%) in identifying severe MR. E wave velocity of 0.9 m/sec had a more optimal combined sensitivity (89%; 95% CI, 74-95%) and specificity (86%; 95% CI, 71-94%). A wave dominance was seen in 18% of case patients and 66% of control subjects (p < 0.001).
CONCLUSION
E wave velocity of 1.2 m/sec is specific not sensitive for severe organic MR; E wave velocity of 0.9 m/sec has better sensitivity and specificity. A wave dominance pattern alone cannot exclude patients with severe organic MR. Our findings highlight the importance of a comprehensive echocardiographic exam rather than relying on a few Doppler parameters in diagnosing MR.
MeSH Terms
Figure
Reference
-
1. Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, Detaint D, Capps M, Nkomo V, Scott C, Schaff HV, Tajik AJ. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med. 2005; 352:875–883.
Article2. Thomas L, Foster E, Schiller NB. Peak mitral inflow velocity predicts mitral regurgitation severity. J Am Coll Cardiol. 1998; 31:174–179.3. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ. American Society of Echocardiography. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802.
Article4. Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, Hagendorff A, Monin JL, Badano L, Zamorano JL. European Association of Echocardiography. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010; 11:307–332.
Article5. Recusani F, Bargiggia GS, Yoganathan AP, Raisaro A, Valdes-Cruz LM, Sung HW, Bertucci C, Gallati M, Moises VA, Simpson IA. A new method for quantification of regurgitant flow rate using color Doppler flow imaging of the flow convergence region proximal to a discrete orifice. An in vitro study. Circulation. 1991; 83:594–604.
Article6. Rodriguez L, Anconina J, Flachskampf FA, Weyman AE, Levine RA, Thomas JD. Impact of finite orifice size on proximal flow convergence.Implications for Doppler quantification of valvular regurgitation. Circ Res. 1992; 70:923–930.
Article7. Rokey R, Sterling LL, Zoghbi WA, Sartori MP, Limacher MC, Kuo LC, Quinones MA. Determination of regurgitant fraction in isolated mitral or aortic regurgitation by pulsed Doppler two-dimensional echocardiography. J Am Coll Cardiol. 1986; 7:1273–1278.
Article8. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Society of Cardiovascular Anesthesiologists. Society for Cardiovascular Angiography and Interventions. Society of Thoracic Surgeons. Bonow RO, Carabello BA, Kanu C, de Leon AC Jr, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT, O'Rourke RA, Otto CM, Shah PM, Shanewise JS, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006; 114:e84–e231.9. Crawford MH, Souchek J, Oprian CA, Miller DC, Rahimtoola S, Giacomini JC, Sethi G, Hammermeister KE. Department of Veterans Affairs Cooperative Study on Valvular Heart Disease. Determinants of survival and left ventricular performance after mitral valve replacement. Circulation. 1990; 81:1173–1181.
Article10. Enriquez-Sarano M, Tajik AJ, Schaff HV, Orszulak TA, McGoon MD, Bailey KR, Frye RL. Echocardiographic prediction of left ventricular function after correction of mitral regurgitation: results and clinical implications. J Am Coll Cardiol. 1994; 24:1536–1543.
Article11. Enriquez-Sarano M, Schaff HV, Orszulak TA, Tajik AJ, Bailey KR, Frye RL. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation. 1995; 91:1022–1028.
Article12. Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). European Association for Cardio-Thoracic Surgery (EACTS). Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schafers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012; 33:2451–2496.
Article13. Appleton CP, Hatle LK, Popp RL. Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol. 1988; 12:426–440.
Article14. Choong CY, Herrmann HC, Weyman AE, Fifer MA. Preload dependence of Doppler-derived indexes of left ventricular diastolic function in humans. J Am Coll Cardiol. 1987; 10:800–808.
Article15. Gardin JM, Davidson DM, Rohan MK, Butman S, Knoll M, Garcia R, Dubria S, Gardin SK, Henry WL. Relationship between age, body size, gender, and blood pressure and Doppler flow measurements in the aorta and pulmonary artery. Am Heart J. 1987; 113:101–109.
Article16. Kuo LC, Quinones MA, Rokey R, Sartori M, Abinader EG, Zoghbi WA. Quantification of atrial contribution to left ventricular filling by pulsed Doppler echocardiography and the effect of age in normal and diseased hearts. Am J Cardiol. 1987; 59:1174–1178.
Article17. Miyatake K, Okamoto M, Kinoshita N, Owa M, Nakasone I, Sakakibara H, Nimura Y. Augmentation of atrial contribution to left ventricular inflow with aging as assessed by intracardiac Doppler flowmetry. Am J Cardiol. 1984; 53:586–589.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Mitral Stenosis by Doppler Echocardiography: Influence of Regurgitation on Doppler Pressure Half-Time
- Echocardiographic Assessment of Mitral Valve Regurgitation
- Congenital Double-Orifice Mitral Valve with Mitral Valve Prolapse and Severe Mitral Regurgitation
- Mitral Valve Repair
- Relationship between Degree of Aortic Regurgitation Graded by 2-D Color Doppler Echocardiography and Diastolic Fluttering of Anterior Mitral Leaflet