J Cardiovasc Ultrasound.
2015 Mar;23(1):1-7. 10.4250/jcu.2015.23.1.1.
Bicuspid Aortic Valve: Unresolved Issues and Role of Imaging Specialists
- Affiliations
-
- 1Asan Medical Center Heart Institute, University of Ulsan College of Medicine, Seoul, Korea. jksong@amc.seoul.kr
- KMID: 2135399
- DOI: http://doi.org/10.4250/jcu.2015.23.1.1
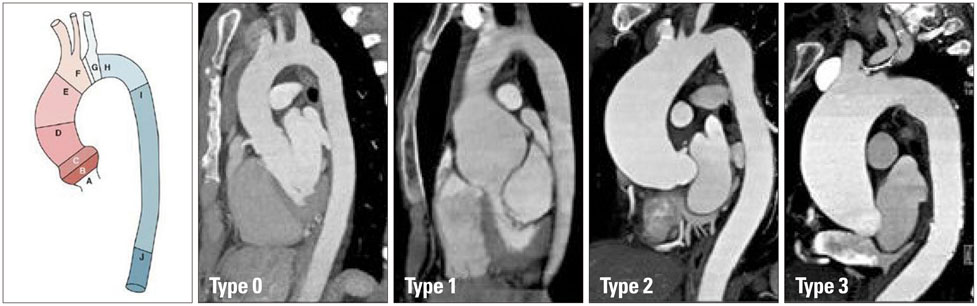
Abstract
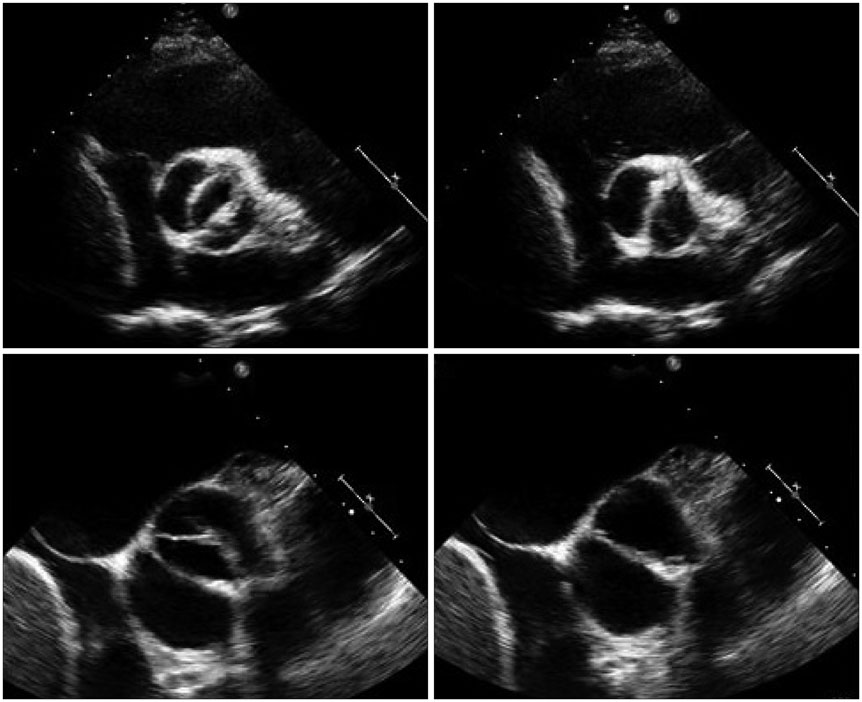
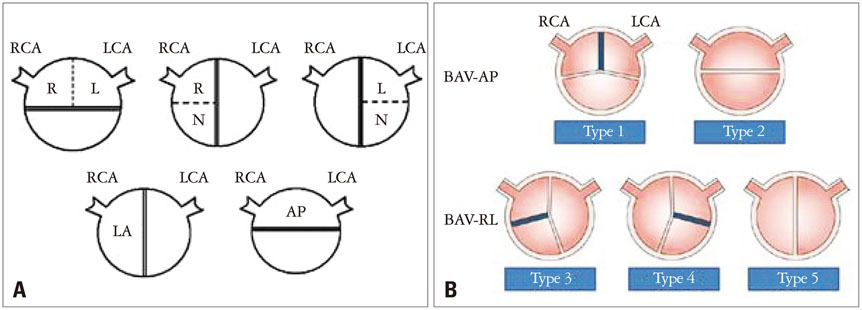
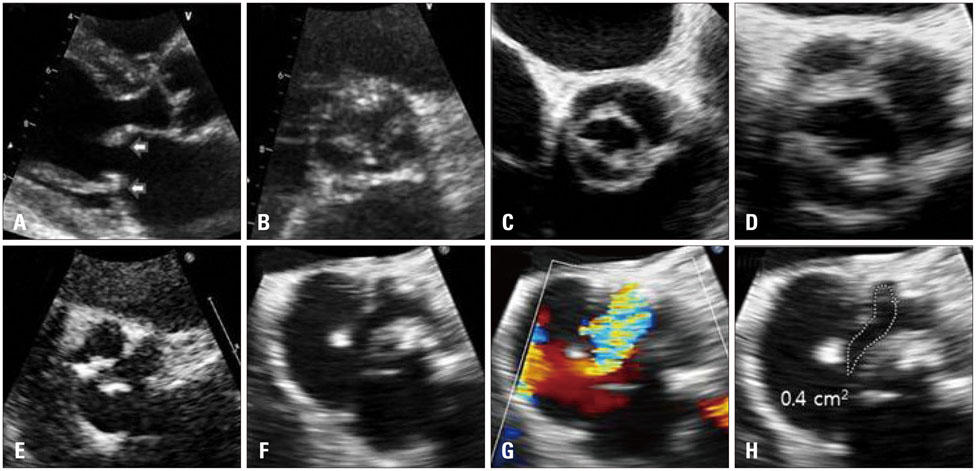
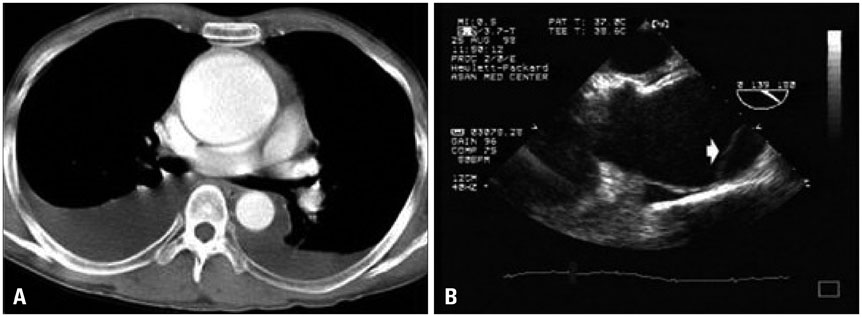
- Bicuspid aortic valve (BAV) is the most common congenital heart disease with marked heterogeneity in many aspects. Fusion patterns of the aortic cusp are quite variable with different type and severity of valvular dysfunction. Moreover, non-valvular cardiovascular abnormalities are associated with BAV. Among them, aortic aneurysm/dissection is the most serious clinical condition with variable patterns of segmental aortic dilatation. Potential association between BAV phenotype and valvulopathy or aortopathy has been suggested, but needs to be tested further. A lack of long-term outcome data at this moment is responsible for unresolved debate regarding appropriate management of patients with BAV, specifically to prevent development of aortic dissection. Long-term follow-up data of a well-characterized cohort or registry based on standardized classification of BAV phenotype and aortopathy are necessary for evidence-based medical practice. Advanced imaging techniques such as computed tomography or magnetic resonance imaging offer better opportunities for accurate phenotype classification and imaging specialists should play a central role to establish a collaborative multicenter cohort or registry.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Timing and Indications for Aortic Valve Surgery in Korean Bicuspid Aortic Valve Patients
Chi Young Shim, Geu-Ru Hong
Korean Circ J. 2018;48(1):82-83. doi: 10.4070/kcj.2017.0380.Mid-term Clinical Outcomes in a Cohort of Asymptomatic or Mildly Symptomatic Korean Patients with Bicuspid Aortic Valve in a Tertiary Referral Hospital
Byung Joo Sun, Jin Kyung Oh, Sun Hack Lee, Jeong Yoon Jang, Ji Hye Lee, Sahmin Lee, Dae-Hee Kim, Jong-Min Song, Duk-Hyun Kang, Jae-Kwan Song
J Cardiovasc Imaging. 2019;27(2):105-118. doi: 10.4250/jcvi.2019.27.e19.
Reference
-
1. Roberts WC. The congenitally bicuspid aortic valve. A study of 85 autopsy cases. Am J Cardiol. 1970; 26:72–83.2. Basso C, Boschello M, Perrone C, Mecenero A, Cera A, Bicego D, Thiene G, De Dominicis E. An echocardiographic survey of primary school children for bicuspid aortic valve. Am J Cardiol. 2004; 93:661–663.
Article3. Nistri S, Basso C, Marzari C, Mormino P, Thiene G. Frequency of bicuspid aortic valve in young male conscripts by echocardiogram. Am J Cardiol. 2005; 96:718–721.
Article4. Siu SC, Silversides CK. Bicuspid aortic valve disease. J Am Coll Cardiol. 2010; 55:2789–2800.
Article5. Michelena HI, Prakash SK, Della Corte A, Bissell MM, Anavekar N, Mathieu P, Bossé Y, Limongelli G, Bossone E, Benson DW, Lancellotti P, Isselbacher EM, Enriquez-Sarano M, Sundt TM 3rd, Pibarot P, Evangelista A, Milewicz DM, Body SC. BAVCon Investigators. Bicuspid aortic valve: identifying knowledge gaps and rising to the challenge from the International Bicuspid Aortic Valve Consortium (BAVCon). Circulation. 2014; 129:2691–2704.6. Schaefer BM, Lewin MB, Stout KK, Gill E, Prueitt A, Byers PH, Otto CM. The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape. Heart. 2008; 94:1634–1638.
Article7. Buchner S, Hülsmann M, Poschenrieder F, Hamer OW, Fellner C, Kobuch R, Feuerbach S, Riegger GA, Djavidani B, Luchner A, Debl K. Variable phenotypes of bicuspid aortic valve disease: classification by cardiovascular magnetic resonance. Heart. 2010; 96:1233–1240.
Article8. Kang JW, Song HG, Yang DH, Baek S, Kim DH, Song JM, Kang DH, Lim TH, Song JK. Association between bicuspid aortic valve phenotype and patterns of valvular dysfunction and bicuspid aortopathy: comprehensive evaluation using MDCT and echocardiography. JACC Cardiovasc Imaging. 2013; 6:150–161.
Article9. Fernández B, Durán AC, Fernández-Gallego T, Fernández MC, Such M, Arqué JM, Sans-Coma V. Bicuspid aortic valves with different spatial orientations of the leaflets are distinct etiological entities. J Am Coll Cardiol. 2009; 54:2312–2318.
Article10. Fernandes SM, Sanders SP, Khairy P, Jenkins KJ, Gauvreau K, Lang P, Simonds H, Colan SD. Morphology of bicuspid aortic valve in children and adolescents. J Am Coll Cardiol. 2004; 44:1648–1651.
Article11. Fernandes SM, Khairy P, Sanders SP, Colan SD. Bicuspid aortic valve morphology and interventions in the young. J Am Coll Cardiol. 2007; 49:2211–2214.
Article12. Braverman AC. Aortic involvement in patients with a bicuspid aortic valve. Heart. 2011; 97:506–513.
Article13. Michelena HI, Khanna AD, Mahoney D, Margaryan E, Topilsky Y, Suri RM, Eidem B, Edwards WD, Sundt TM 3rd, Enriquez-Sarano M. Incidence of aortic complications in patients with bicuspid aortic valves. JAMA. 2011; 306:1104–1112.
Article14. Kim YG, Sun BJ, Park GM, Han S, Kim DH, Song JM, Kang DH, Song JK. Aortopathy and bicuspid aortic valve: haemodynamic burden is main contributor to aortic dilatation. Heart. 2012; 98:1822–1827.
Article15. Hahn RT, Roman MJ, Mogtader AH, Devereux RB. Association of aortic dilation with regurgitant, stenotic and functionally normal bicuspid aortic valves. J Am Coll Cardiol. 1992; 19:283–288.
Article16. Keane MG, Wiegers SE, Plappert T, Pochettino A, Bavaria JE, Sutton MG. Bicuspid aortic valves are associated with aortic dilatation out of proportion to coexistent valvular lesions. Circulation. 2000; 102:19 Suppl 3. III35–III39.
Article17. Beroukhim RS, Kruzick TL, Taylor AL, Gao D, Yetman AT. Progression of aortic dilation in children with a functionally normal bicuspid aortic valve. Am J Cardiol. 2006; 98:828–830.
Article18. Della Corte A, Bancone C, Quarto C, Dialetto G, Covino FE, Scardone M, Caianiello G, Cotrufo M. Predictors of ascending aortic dilatation with bicuspid aortic valve: a wide spectrum of disease expression. Eur J Cardiothorac Surg. 2007; 31:397–404. discussion 404-5.
Article19. Yasuda H, Nakatani S, Stugaard M, Tsujita-Kuroda Y, Bando K, Kobayashi J, Yamagishi M, Kitakaze M, Kitamura S, Miyatake K. Failure to prevent progressive dilation of ascending aorta by aortic valve replacement in patients with bicuspid aortic valve: comparison with tricuspid aortic valve. Circulation. 2003; 108:Suppl 1. II291–II294.
Article20. Huntington K, Hunter AG, Chan KL. A prospective study to assess the frequency of familial clustering of congenital bicuspid aortic valve. J Am Coll Cardiol. 1997; 30:1809–1812.
Article21. Cripe L, Andelfinger G, Martin LJ, Shooner K, Benson DW. Bicuspid aortic valve is heritable. J Am Coll Cardiol. 2004; 44:138–143.
Article22. Garg V, Muth AN, Ransom JF, Schluterman MK, Barnes R, King IN, Grossfeld PD, Srivastava D. Mutations in NOTCH1 cause aortic valve disease. Nature. 2005; 437:270–274.
Article23. Mohamed SA, Aherrahrou Z, Liptau H, Erasmi AW, Hagemann C, Wrobel S, Borzym K, Schunkert H, Sievers HH, Erdmann J. Novel missense mutations (p.T596M and p.P1797H) in NOTCH1 in patients with bicuspid aortic valve. Biochem Biophys Res Commun. 2006; 345:1460–1465.
Article24. Forte A, Della Corte A, Grossi M, Bancone C, Provenzano R, Finicelli M, De Feo M, De Santo LS, Nappi G, Cotrufo M, Galderisi U, Cipollaro M. Early cell changes and TGFβ pathway alterations in the aortopathy associated with bicuspid aortic valve stenosis. Clin Sci (Lond). 2013; 124:97–108.
Article25. Charitos EI, Stierle U, Petersen M, Mohamed SA, Hanke T, Schmidtke C, Klotz S, Sievers HH. The fate of the bicuspid valve aortopathy after aortic valve replacement. Eur J Cardiothorac Surg. 2014; 45:e128–e135.
Article26. Kari FA, Fazel SS, Mitchell RS, Fischbein MP, Miller DC. Bicuspid aortic valve configuration and aortopathy pattern might represent different pathophysiologic substrates. J Thorac Cardiovasc Surg. 2012; 144:516–517.
Article27. Della Corte A, Bancone C, Dialetto G, Covino FE, Manduca S, Montibello MV, De Feo M, Buonocore M, Nappi G. The ascending aorta with bicuspid aortic valve: a phenotypic classification with potential prognostic significance. Eur J Cardiothorac Surg. 2014; 46:240–247. discussion 247.
Article28. Hope MD, Hope TA, Meadows AK, Ordovas KG, Urbania TH, Alley MT, Higgins CB. Bicuspid aortic valve: four-dimensional MR evaluation of ascending aortic systolic flow patterns. Radiology. 2010; 255:53–61.
Article29. Mahadevia R, Barker AJ, Schnell S, Entezari P, Kansal P, Fedak PW, Malaisrie SC, McCarthy P, Collins J, Carr J, Markl M. Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. Circulation. 2014; 129:673–682.
Article30. Michelena HI, Desjardins VA, Avierinos JF, Russo A, Nkomo VT, Sundt TM, Pellikka PA, Tajik AJ, Enriquez-Sarano M. Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community. Circulation. 2008; 117:2776–2784.
Article31. Tzemos N, Therrien J, Yip J, Thanassoulis G, Tremblay S, Jamorski MT, Webb GD, Siu SC. Outcomes in adults with bicuspid aortic valves. JAMA. 2008; 300:1317–1325.
Article32. Hardikar AA, Marwick TH. Surgical thresholds for bicuspid aortic valve associated aortopathy. JACC Cardiovasc Imaging. 2013; 6:1311–1320.
Article33. Kallenbach K, Sundt TM, Marwick TH. Aortic surgery for ascending aortic aneurysms under 5.0 cm in diameter in the presence of bicuspid aortic valve. JACC Cardiovasc Imaging. 2013; 6:1321–1326.
Article34. Verma S, Yanagawa B, Kalra S, Ruel M, Peterson MD, Yamashita MH, Fagan A, Currie ME, White CW, Wai Sang SL, Rosu C, Singh S, Mewhort H, Gupta N, Fedak PW. Knowledge, attitudes, and practice patterns in surgical management of bicuspid aortopathy: a survey of 100 cardiac surgeons. J Thorac Cardiovasc Surg. 2013; 146:1033–1040.e4.
Article35. Barker AJ, Robinson JD, Markl M. Bicuspid aortic valve phenotype and aortopathy: nomenclature and role of aortic hemodynamics. JACC Cardiovasc Imaging. 2013; 6:921.
Article36. Della Corte A. Phenotypic heterogeneity of bicuspid aortopathy: a potential key to decode the prognosis? Heart. 2014; 100:96–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ascending Aortic Aneurysm Associated with Congenital Bicuspid Aortic Valve
- Aortic Coarctation Following Aortic Valve Replacement: Problem Solving with Multimodality Cardiac Imaging
- Ruptured Subvalvular Aortic Aneurysm of a Person Who Has Bicuspid Aortic Valve
- Understanding the Natural History of Bicuspid Aortic Valve: Are We Close to Understanding It?
- A Case of Double Orifice Mitral Valve in a Patient with Bicuspid Aortic Valve: Coincidental or a Missed Finding?