Electrolyte Blood Press.
2007 Jun;5(1):1-8. 10.5049/EBP.2007.5.1.1.
Clinical Significance of Strong Ion Gap: between ICU and Hemodialysis Patients with Metabolic Acidosis
- Affiliations
-
- 1Department of Internal Medicine, Eulji University Hospital, Daejeon, Korea. visionjcys@eulji.ac.kr
- KMID: 2134798
- DOI: http://doi.org/10.5049/EBP.2007.5.1.1
Abstract
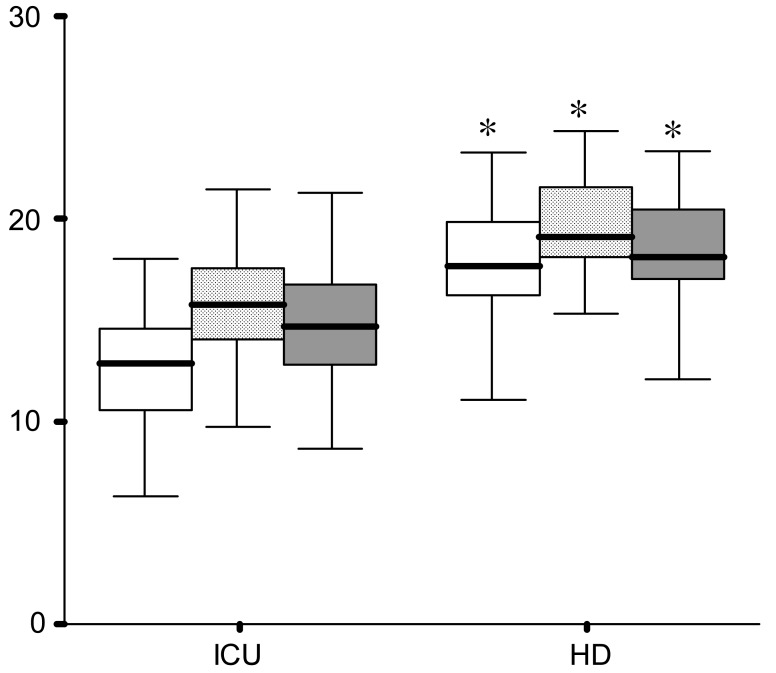
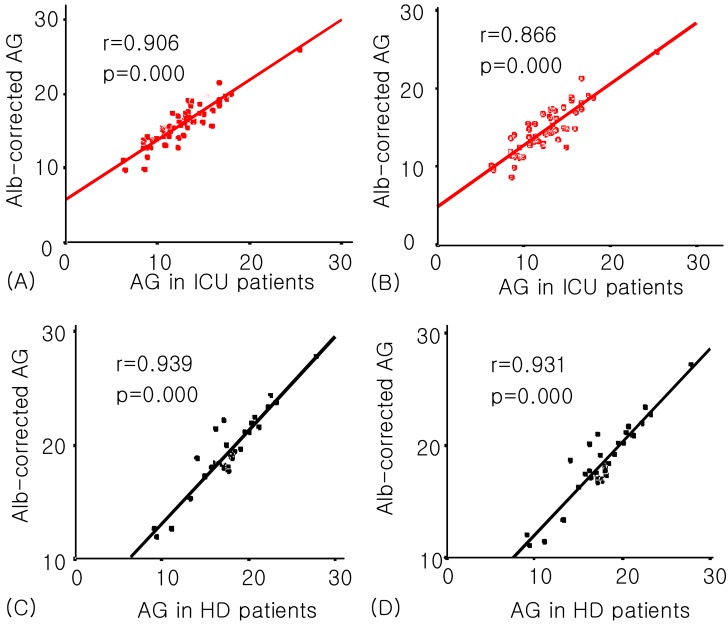
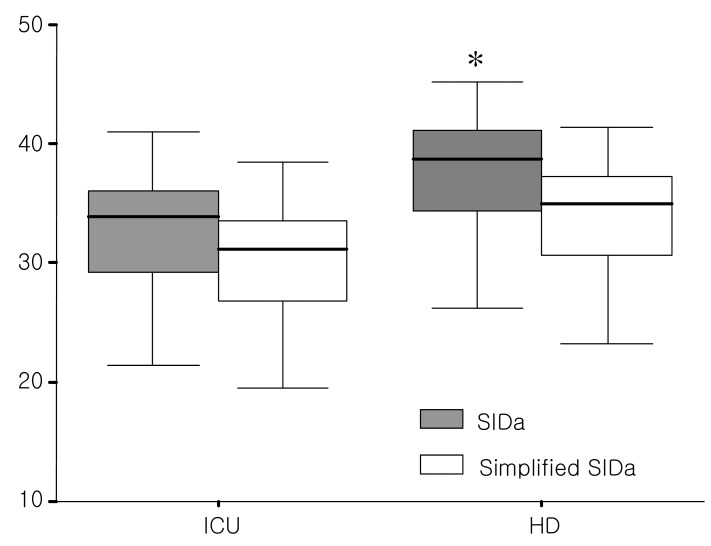
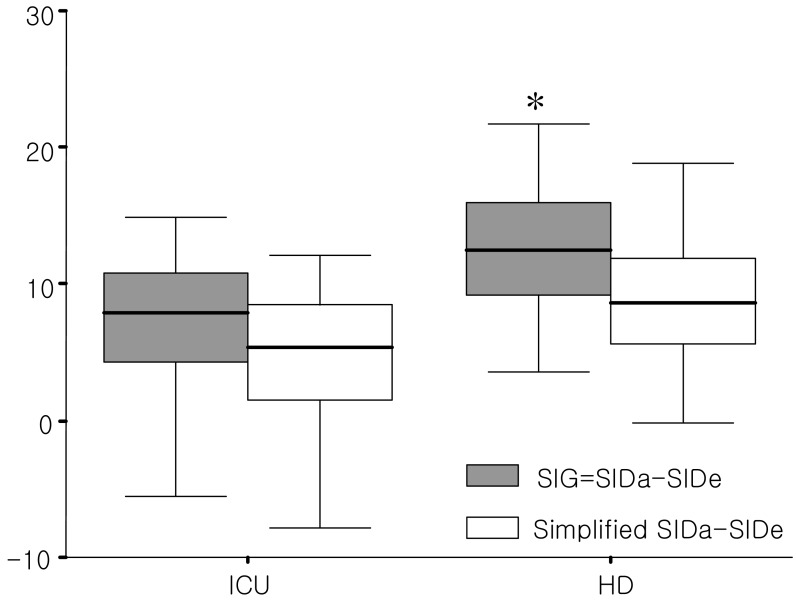
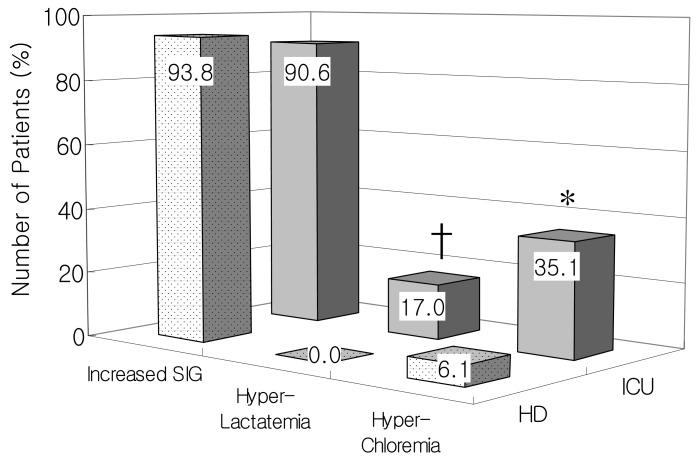
- Metabolic acidosis is the most frequent acid-base disorder in critically ill patients and dialysis patients. This study is to compare the conventional approach with the physicochemical approach between the intensive care unit (ICU) and hemodialysis (HD) patients. Fifty-seven ICU patients and 33 HD patients were enrolled. All data sets included simultaneous measurements of arterial blood gas with base deficit (BD), serum electrolytes, albumin, lactate, and calculated anion gap observed (AGobs). Physiochemical analysis was used to calculate the albumin and lactate-corrected anion gap (AGcorr), the base deficit corrected for unmeasured anions (BDua), the strong ion difference apparent (SIDa), the strong ion difference effective (SIDe), and the strong ion gap (SIG). The SIDa (37.5+/-5.3 vs 33.9+/-9.0, p=0.045) and SIG (12.3+/-5.3 vs 8.6+/-8.8, p=0.043) was significantly higher in the HD group than the ICU group. SIG in the ICU group showed the highest correlation coefficient with AGobs, whereas SIG in the HD group with AGcorr. Concerning the contributions of the three main causes of metabolic acidosis, increased SIG was comparable between the ICU and HD group (n=48, 90.6% vs n=30, 93.8%), whereas hyperlactatemia (n=9, 17.0% vs n=0, 0%) and hyperchloremia (n=20, 35.1% vs n=2, 6.1%) was significantly increased in the ICU group compared with the HD group. Multiple underlying mechanisms are present in most of the ICU patients with metabolic acidosis compared with the HD patients. In conclusion, the physicochemical approach can elucidate the detailed mechanisms of metabolic acidosis in ICU and HD patients compared with conventional measures.
MeSH Terms
Figure
Reference
-
1. Rehm M, Conzen PF, Peter K, Finsterer U. [The Stewart model. "Modern" approach to the interpretation of the acid-base metabolism]. Anaesthesist. 2004; 53:347–357. PMID: 15088097.2. Morgan TJ. The meaning of acid-base abnormalities in the intensive care unit: part III - effects of fluid administration. Crit Care. 2005; 9:204–211. PMID: 15774079.3. Schuck O, Matousovic K. Relation between pH and the strong ion difference (SID) in body fluids. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2005; 149:69–73. PMID: 16170391.4. Carreira F, Anderson RJ. Assessing metabolic acidosis in the intensive care unit : does the method make a difference? Crit Care Med. 2004; 32:1227–1228. PMID: 15190979.5. Kellum JA, Kramer DJ, Pinsky MR. Strong ion gap : a methodology for exploring unexplained anions. J Crit Care. 1995; 10:51–55. PMID: 7647842.6. Moviat M, van Haren F, van der Hoeven H. Conventional or physicochemical approach in intensive care unit patients with metabolic acidosis. Crit Care. 2003; 7:R41–R45. PMID: 12793889.7. Rocktaeschel J, Morimatsu H, Uchino S, Bellomo R. Unmeasured anions in critically ill patients : can they predict mortality? Crit Care Med. 2003; 31:2131–2136. PMID: 12973170.8. Cole L, Bellomo R, Baldwin I, Hayhoe M, Ronco C. The impact of lactate-buffered high-volume hemofiltration on acid-base balance. Intensive Care Med. 2003; 29:1113–1120. PMID: 12783161.
Article9. Bruegger D, Jacob M, Scheingraber S, Conzen P, Becker BF, Finsterer U, Rehm M. Changes in acid-base balance following bolus infusion of 20% albumin solution in humans. Intensive Care Med. 2005; 31:1123–1127. PMID: 15999255.
Article10. Moviat M, Pickkers P, van der Voort PH, van der Hoeven JG. Acetazolamide-mediated decrease in strong ion difference accounts for the correction of metabolic alkalosis in critically ill patients. Crit Care. 2006; 10:R14. PMID: 16420662.11. Naka T, Bellomo R. Bench-to-bedside review : treating acid-base abnormalities in the intensive care unit-the role of renal replacement therapy. Crit Care. 2004; 8:108–114. PMID: 15025771.12. Levraut J, Grimaud D. Treatment of metabolic acidosis. Curr Opin Crit Care. 2003; 9:260–265. PMID: 12883279.
Article13. Oh MS, Uribarri J, Weinstein J, Schreiber M, Kamel KS, Kraut JA, Madias NE, Laski ME. What unique acid-base considerations exist in dialysis patients? Semin Dial. 2004; 17:351–364. PMID: 15461741.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ethylene Glycol Poisoning with Metabolic Acidosis Treated with Hemodialysis
- Acid-Base Disorders in ICU Patients
- Acid-base changes during liver transplantation using Stewart's physicochemical approach: living related donor vs. cadaveric donor
- A Case of Metformin-Induced Acute Kidney Injury without Lactic Acidosis: A Case Report
- Metabolic acidosis and abnormal calcium metabolism in patients on maintenance hemodialysis