Clin Endosc.
2012 Sep;45(3):235-239.
Esophageal Stent for Cervical Esophagus and Esophagogastric Junction
- Affiliations
-
- 1Digestive Disease Center, Konkuk University Medical Center, Seoul, Korea. chansshim@naver.com
Abstract
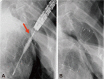
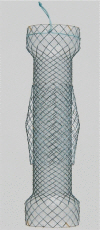
- Tumors in the cervical portion of the esophagus have traditionally been more difficult to manage. The implantation in the cervical esophagus is a technically demanding procedure. The implantation of modified self-expandable metal stents (SEMSs) was very effective perorally under endoscopic and fluoroscopic guidance. Experience with SEMS has revealed an increased risk of migration when either covered stents are used or a stent is implanted across the gastroesophageal junction. The modified, covered, esophageal stents appear to prevent stent migration and improve dysphagia in patients with malignant tumor stenosis at the esophagogastric junction. Besides heartburn, regurgitation is sometimes very distressing to patients and may lead to fatal aspiration due to reflux after stenting in esophagogastric junction. These symptoms can be reduced by the use of valved stent. The long S-shape valve is very effective in preventing acid reflux and valve inversion.
MeSH Terms
Figure
Reference
-
1. Shields SJ. Esophageal self-expandable metallic stents. Gastrointest Endosc. 1997; 45:439–442. PMID: 9165334.
Article2. Macdonald S, Edwards RD, Moss JG. Patient tolerance of cervical esophageal metallic stents. J Vasc Interv Radiol. 2000; 11:891–898. PMID: 10928528.
Article3. Shim CS, Jung IS, Bhandari S, et al. Management of malignant strictures of the cervical esophagus with a newly-designed self-expanding metal stent. Endoscopy. 2004; 36:554–557. PMID: 15202054.
Article4. Kozarek RA, Raltz S, Brugge WR, et al. Prospective multicenter trial of esophageal Z-stent placement for malignant dysphagia and tracheoesophageal fistula. Gastrointest Endosc. 1996; 44:562–567. PMID: 8934162.
Article5. Shim CS, Cho YD, Moon JH, et al. Fixation of a modified covered esophageal stent: its clinical usefulness for preventing stent migration. Endoscopy. 2001; 33:843–848. PMID: 11571679.
Article6. Verschuur EM, Homs MY, Steyerberg EW, et al. A new esophageal stent design (Niti-S stent) for the prevention of migration: a prospective study in 42 patients. Gastrointest Endosc. 2006; 63:134–140. PMID: 16377330.
Article7. Dua KS, Kozarek R, Kim J, et al. Self-expanding metal esophageal stent with anti-reflux mechanism. Gastrointest Endosc. 2001; 53:603–613. PMID: 11323586.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Covered Nitinol Stent Fracture in a Patient with a Malignant Esophageal Stricture: A Case Report
- Current and Future Use of Esophageal Capsule Endoscopy
- Diagnostic Approach for Esophagogastric Junction Outflow Obstruction
- A Case of Double Primary Cancer that Occurred Continuously at the Esophagogastric Junction
- Leiomyoma in the Esophagogastric Junction Removed by Enucleation