Yonsei Med J.
2014 Jul;55(4):1095-1100. 10.3349/ymj.2014.55.4.1095.
Concentration of Non-Steroidal Anti-Inflammatory Drugs in the Pelvic Floor Muscles: An Experimental Comparative Rat Model
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Taipei Medical University Hospital, Taipei, Taiwan.
- 2Department of Obstetrics and Gynecology, Chang Gung Memorial Hospital at Keelung, Keelung, Taiwan.
- 3Department of Research and Development, Standard Chemistry and Pharmaceutical. Co., Ltd, Taipei, Taiwan.
- 4Department of Bioanalysis, Standard Chemistry and Pharmaceutical. Co., Ltd, Taipei, Taiwan.
- 5Department of Obstetrics and Gynecology, Chang Gung Memorial Hospital at Linkou and Chang Gung University College of Medicine, Tao-Yuan, Taiwan. wang2260@gmail.com
- KMID: 2130838
- DOI: http://doi.org/10.3349/ymj.2014.55.4.1095
Abstract
- PURPOSE
The aim of this study is to explore non-steroid anti-inflammation drugs (NSAIDs) potency for pelvic floor muscle pain by measuring local concentration in a rat model.
MATERIALS AND METHODS
We used nine NSAIDs, including nabumetone, naproxen, ibuprofen, meloxicam, piroxicam, diclofenac potassium, etodolac, indomethacin, and sulindac, and 9 groups of female Wister rats. Each group of rats was fed with one kind of NSAID (2 mg/mL) for three consecutive days. Thereafter, one mL of blood and one gram of pelvic floor muscle were taken to measure drug pharmacokinetics, including partition coefficient, lipophilicity, elimination of half-life (T1/2) and muscle/plasma converting ratio (Css, muscle/Css, plasma).
RESULTS
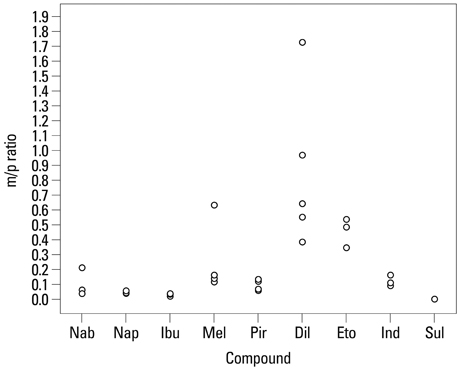
Diclofenac potassium had the lowest T1/2 and the highest mean Css, muscle/Css, plasma (1.9 hours and 0.85+/-0.53, respectively). The mean Css, muscle/Css, plasma of sulindac, naproxen and ibuprofen were lower than other experimental NSAIDs.
CONCLUSION
Diclofenac potassium had the highest disposition in pelvic floor muscle in a rat model. The finding implies that diclofenac potassium might be the choice for pain relief in pelvic muscle.
Keyword
MeSH Terms
-
Animals
Anti-Inflammatory Agents, Non-Steroidal/*therapeutic use
Butanones/therapeutic use
Chronic Pain/*drug therapy
Diclofenac/therapeutic use
Female
Muscles/drug effects
Naproxen/therapeutic use
Pelvic Floor/*pathology
Pelvic Pain/*drug therapy
Piroxicam/therapeutic use
Rats
Rats, Wistar
Thiazines/therapeutic use
Thiazoles/therapeutic use
Anti-Inflammatory Agents, Non-Steroidal
Butanones
Thiazines
Thiazoles
Piroxicam
Diclofenac
Naproxen
Figure
Reference
-
1. Zondervan KT, Yudkin PL, Vessey MP, Dawes MG, Barlow DH, Kennedy SH. Prevalence and incidence of chronic pelvic pain in primary care: evidence from a national general practice database. Br J Obstet Gynaecol. 1999; 106:1149–1155.
Article2. Howard FM. The role of laparoscopy in chronic pelvic pain: promise and pitfalls. Obstet Gynecol Surv. 1993; 48:357–387.
Article3. Vercellini P, Viganò P, Somigliana E, Abbiati A, Barbara G, Fedele L. Medical, surgical and alternative treatments for chronic pelvic pain in women: a descriptive review. Gynecol Endocrinol. 2009; 25:208–221.
Article4. Lee NC, Dicker RC, Rubin GL, Ory HW. Confirmation of the preoperative diagnoses for hysterectomy. Am J Obstet Gynecol. 1984; 150:283–287.
Article5. Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Engl J Med. 1993; 328:856–860.
Article6. Krames E. Using a pain treatment continuum: a logical and cost-effective approach. In : Raj PP, editor. Practical Management of Pain. St. Louis: Mosby;2000. p. 441–444.7. Owen PR. Prostaglandin synthetase inhibitors in the treatment of primary dysmenorrhea. Outcome trials reviewed. Am J Obstet Gynecol. 1984; 148:96–103.
Article8. Zhang WY, Li Wan Po A. Efficacy of minor analgesics in primary dysmenorrhoea: a systematic review. Br J Obstet Gynaecol. 1998; 105:780–789.
Article9. Akin MD, Weingand KW, Hengehold DA, Goodale MB, Hinkle RT, Smith RP. Continuous low-level topical heat in the treatment of dysmenorrhea. Obstet Gynecol. 2001; 97:343–349.
Article10. Budoff PW. Use of mefenamic acid in the treatment of primary dysmenorrhea. JAMA. 1979; 241:2713–2716.
Article11. Milsom I, Minic M, Dawood MY, Akin MD, Spann J, Niland NF, et al. Comparison of the efficacy and safety of nonprescription doses of naproxen and naproxen sodium with ibuprofen, acetaminophen, and placebo in the treatment of primary dysmenorrhea: a pooled analysis of five studies. Clin Ther. 2002; 24:1384–1400.
Article12. Hillis SD, Marchbanks PA, Peterson HB. The effectiveness of hysterectomy for chronic pelvic pain. Obstet Gynecol. 1995; 86:941–945.
Article13. Prather H, Dugan S, Fitzgerald C, Hunt D. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM R. 2009; 1:346–358.
Article14. Baker PK. Musculoskeletal origins of chronic pelvic pain. Diagnosis and treatment. Obstet Gynecol Clin North Am. 1993; 20:719–742.15. Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol. 2001; 166:2226–2231.
Article16. Glazer HI, Rodke G, Swencionis C, Hertz R, Young AW. Treatment of vulvar vestibulitis syndrome with electromyographic biofeedback of pelvic floor musculature. J Reprod Med. 1995; 40:283–290.
Article17. Lukban J, Whitmore K, Kellogg-Spadt S, Bologna R, Lesher A, Fletcher E. The effect of manual physical therapy in patients diagnosed with interstitial cystitis, high-tone pelvic floor dysfunction, and sacroiliac dysfunction. Urology. 2001; 57:6 Suppl 1. 121–122.
Article18. Sinaki M, Merritt JL, Stillwell GK. Tension myalgia of the pelvic floor. Mayo Clin Proc. 1977; 52:717–722.19. Gunter J. Chronic pelvic pain: an integrated approach to diagnosis and treatment. Obstet Gynecol Surv. 2003; 58:615–623.
Article20. Thiele GH. Coccygodynia: cause and treatment. Dis Colon Rectum. 1963; 6:422–436.21. Panchagnula R, Thomas NS. Biopharmaceutics and pharmacokinetics in drug research. Int J Pharm. 2000; 201:131–150.
Article22. Ho RH, Kim RB. Transporters and drug therapy: implications for drug disposition and disease. Clin Pharmacol Ther. 2005; 78:260–277.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Updates of Spondyloarthrothy Treatment
- Current Guidelines for Non-Steroidal Anti-Inflammatory Drugs
- The Efficacy of Pelvic Floor Muscles Exercise Combined with Biofeedback and Electrical Stimulation in Recurred Stress In continence or Intrinsic Sphincter Dysfunction Patients
- Experimental study of the effects of non-steroidal anti-inflammatory agents used in dental clinic on orthodontic tooth movement in rats
- Diagnosis and treatment of Helicobacter pylori infection in patients treated with non-steroidal anti-inflammatory drugs