Yonsei Med J.
2014 Jul;55(4):1072-1079. 10.3349/ymj.2014.55.4.1072.
Cervical Arthroplasty for Moderate to Severe Disc Degeneration: Clinical and Radiological Assessments after a Minimum Follow-Up of 18 Months: Pfirrmann Grade and Cervical Arthroplasty
- Affiliations
-
- 1Department of Neurosurgery, Guro Teun Teun Hospital, Seoul, Korea.
- 2Department of Neurosurgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 3Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Radiology, Inha University Hospital, Incheon, Korea.
- 5Department of Neurosurgery, Inha University Hospital, Incheon, Korea. nsyoon@gmail.com
- KMID: 2130835
- DOI: http://doi.org/10.3349/ymj.2014.55.4.1072
Abstract
- PURPOSE
Clinical outcomes and radiologic results after cervical arthroplasty have been reported in many articles, yet relatively few studies after cervical arthroplasty have been conducted in severe degenerative cervical disc disease.
MATERIALS AND METHODS
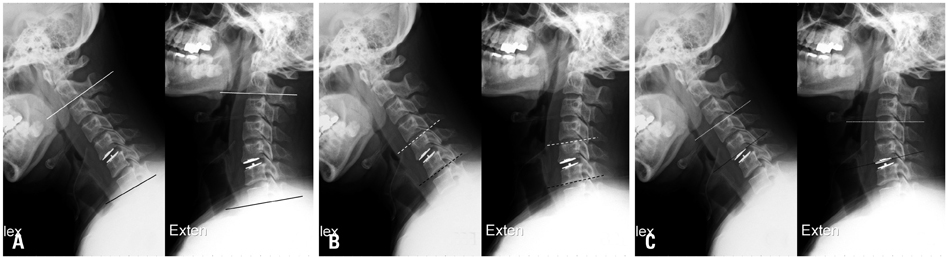
Sixty patients who underwent cervical arthroplasty (Mobi-C(R)) between April 2006 and November 2011 with a minimum follow-up of 18 months were enrolled in this study. Patients were divided into two groups according to Pfirrmann classification on preoperative cervical MR images: group A (Pfirrmann disc grade III, n=38) and group B (Pfirrmann disc grades IV or V, n=22). Visual analogue scale (VAS) scores of neck and arm pain, modified Oswestry Disability Index (mODI) score, and radiological results including cervical range of motion (ROM) were assessed before and after surgery.
RESULTS
VAS and mean mODI scores decreased after surgery from 5.1 and 57.6 to 2.7 and 31.5 in group A and from 6.1 and 59.9 to 3.7 and 38.4 in group B, respectively. In both groups, VAS and mODI scores significantly improved postoperatively (p<0.001), although no significant intergroup differences were found. Also, cervical dynamic ROM was preserved or gradually improved up to 18 months after cervical arthroplasty in both groups. Global, segmental and adjacent ROM was similar for both groups during follow-up. No cases of device subsidence or extrusion were recorded.
CONCLUSION
Clinical and radiological results following cervical arthroplasty in patients with severe degenerative cervical disc disease were no different from those in patients with mild degenerative cervical disc disease after 18 months of follow-up.
Keyword
MeSH Terms
Figure
Reference
-
1. Agrillo U, Faccioli F, Fachinetti P, Gambardella G, Guizzardi G, Profeta G. Guidelines for the diagnosis and management of the degenerative diseases of cervical spine. J Neurosurg Sci. 1999; 43:11–14.2. Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine (Phila Pa 1976). 1984; 9:667–671.3. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40-A:607–624.
Article4. Wigfield C, Gill S, Nelson R, Langdon I, Metcalf N, Robertson J. Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disc disease. J Neurosurg. 2002; 96:1 Suppl. 17–21.
Article5. Anderson PA, Rouleau JP. Intervertebral disc arthroplasty. Spine (Phila Pa 1976). 2004; 29:2779–2786.
Article6. Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007; 6:198–209.
Article7. Park JH, Roh KH, Cho JY, Ra YS, Rhim SC, Noh SW. Comparative analysis of cervical arthroplasty using mobi-c(r) and anterior cervical discectomy and fusion using the solis(r)-cage. J Korean Neurosurg Soc. 2008; 44:217–221.
Article8. Yoon DH, Yi S, Shin HC, Kim KN, Kim SH. Clinical and radiological results following cervical arthroplasty. Acta Neurochir (Wien). 2006; 148:943–950.
Article9. Jacobs B, Krueger EG, Leivy DM. Cervical spondylosis with radiculopathy. Results of anterior diskectomy and interbody fusion. JAMA. 1970; 211:2135–2139.
Article10. Nabhan A, Ahlhelm F, Shariat K, Pitzen T, Steimer O, Steudel WI, et al. The ProDisc-C prosthesis: clinical and radiological experience 1 year after surgery. Spine (Phila Pa 1976). 2007; 32:1935–1941.11. Sekhon LH. Cervical arthroplasty in the management of spondylotic myelopathy: 18-month results. Neurosurg Focus. 2004; 17:E8.
Article12. Wang Y, Zhang X, Xiao S, Lu N, Wang Z, Zhou M. Clinical report of cervical arthroplasty in management of spondylotic myelopathy in Chinese. J Orthop Surg Res. 2006; 1:13.
Article13. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26:1873–1878.
Article14. Takatalo J, Karppinen J, Taimela S, Niinimäki J, Laitinen J, Sequeiros RB, et al. Association of abdominal obesity with lumbar disc degeneration--a magnetic resonance imaging study. PLoS One. 2013; 8:e56244.15. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999; 81:519–528.
Article16. Shin DA, Yi S, Yoon DH, Kim KN, Shin HC. Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine (Phila Pa 1976). 2009; 34:1153–1159.
Article17. Kim DY, Oh CH, Yoon SH, Park HC, Park CO. Lumbar disc screening using Back Pain Questionnaires: Oswestry Low Back Pain Score, Aberdeen Low Back Pain Scale, and Acute Low Back Pain Screening Questionnaire. Korean J Spine. 2012; 9:153–158.
Article18. Cherubino P, Benazzo F, Borromeo U, Perle S. Degenerative arthritis of the adjacent spinal joints following anterior cervical spinal fusion: clinicoradiologic and statistical correlations. Ital J Orthop Traumatol. 1990; 16:533–543.19. Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J. Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine. 2007; 7:33–39.
Article20. Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001; 10:320–324.
Article21. Döhler JR, Kahn MR, Hughes SP. Instability of the cervical spine after anterior interbody fusion. A study on its incidence and clinical significance in 21 patients. Arch Orthop Trauma Surg. 1985; 104:247–250.22. Hunter LY, Braunstein EM, Bailey RW. Radiographic changes following anterior cervical fusion. Spine (Phila Pa 1976). 1980; 5:399–401.
Article23. McGrory BJ, Klassen RA. Arthrodesis of the cervical spine for fractures and dislocations in children and adolescents. A long-term follow-up study. J Bone Joint Surg Am. 1994; 76:1606–1616.
Article24. Davis RJ, Kim KD, Hisey MS, Hoffman GA, Bae HW, Gaede SE, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial: clinical article. J Neurosurg Spine. 2013; 19:532–545.
Article25. Chen Y, Wang X, Lu X, Yang H, Chen D. Cervical disk arthroplasty versus ACDF for preoperative reducible kyphosis. Orthopedics. 2013; 36:e958–e965.
Article26. Phillips FM, Lee JY, Geisler FH, Cappuccino A, Chaput CD, DeVine JG, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion 2-year results from the US FDA IDE clinical trial. Spine (Phila Pa 1976). 2013; 38:E907–E918.27. Verma K, Gandhi SD, Maltenfort M, Albert TJ, Hilibrand AS, Vaccaro AR, et al. Rate of adjacent segment disease in cervical disc arthroplasty versus single-level fusion: meta-analysis of prospective studies. Spine (Phila Pa 1976). 2013; 38:2253–2257.
Article28. Yin S, Yu X, Zhou S, Yin Z, Qiu Y. Is cervical disc arthroplasty superior to fusion for treatment of symptomatic cervical disc disease? A meta-analysis. Clin Orthop Relat Res. 2013; 471:1904–1919.
Article29. Goffin J, van Loon J, Van Calenbergh F, Lipscomb B. A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan Cervical Disc Prosthesis. J Neurosurg Spine. 2010; 12:261–269.
Article30. Huppert J, Beaurain J, Steib JP, Bernard P, Dufour T, Hovorka I, et al. Comparison between single- and multi-level patients: clinical and radiological outcomes 2 years after cervical disc replacement. Eur Spine J. 2011; 20:1417–1426.
Article31. Zweig T, Hemmeler C, Aghayev E, Melloh M, Etter C, Röder C. Influence of preoperative nucleus pulposus status and radiculopathy on outcomes in mono-segmental lumbar total disc replacement: results from a nationwide registry. BMC Musculoskelet Disord. 2011; 12:275.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Cervical Disc Replacement using Artificial Disc in Cervical Disc Herniations
- Quantitative Pfirrmann Disc Degeneration Grading System to Overcome the Limitation of Pfirrmann Disc Degeneration Grade
- Comparative Analysis of Cervical Arthroplasty Using Mobi-C(R) and Anterior Cervical Discectomy and Husion Using the Solis(R) -Cage
- Early Radiological Analysis of Cervical Arthroplasty with Bryan and Mobi-C Cervical Disc Prosthesis
- Whole Spine Disc Degeneration Survey according to the Ages and Sex Using Pfirrmann Disc Degeneration Grades