Yonsei Med J.
2014 Jul;55(4):928-936. 10.3349/ymj.2014.55.4.928.
Early Repolarization and Myocardial Scar Predict Poorest Prognosis in Patients with Coronary Artery Disease
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- 2Division of Cardiology, Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2130816
- DOI: http://doi.org/10.3349/ymj.2014.55.4.928
Abstract
- PURPOSE
Recent studies show positive association of early repolarization (ER) with the risk of life-threatening arrhythmias in patients with coronary artery disease (CAD). This study was to investigate the relationships of ER with myocardial scarring and prognosis in patients with CAD.
MATERIALS AND METHODS
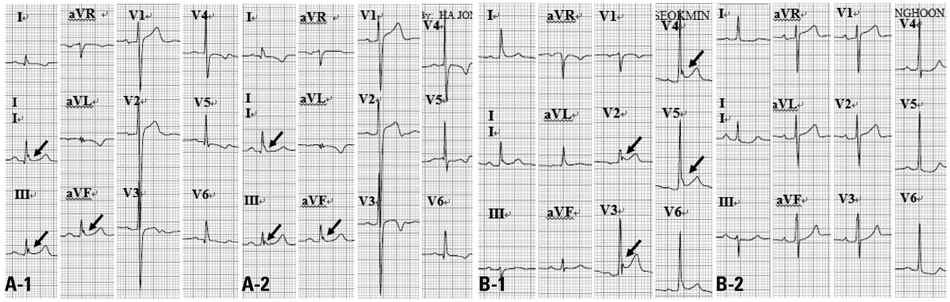
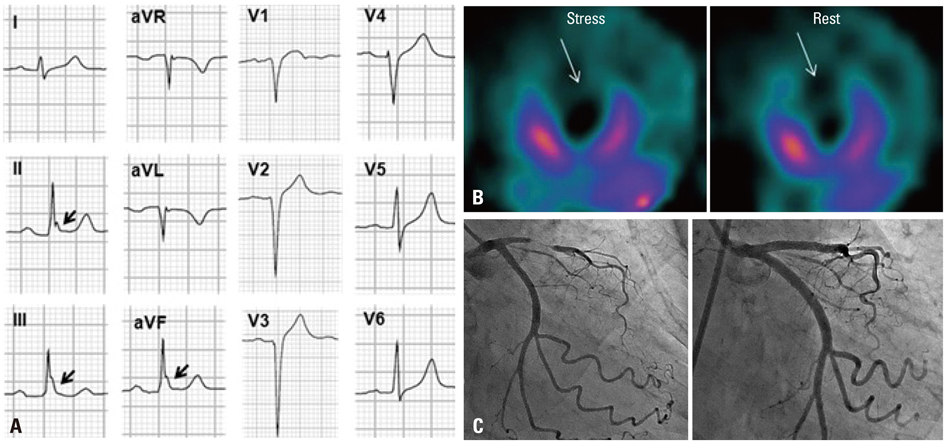
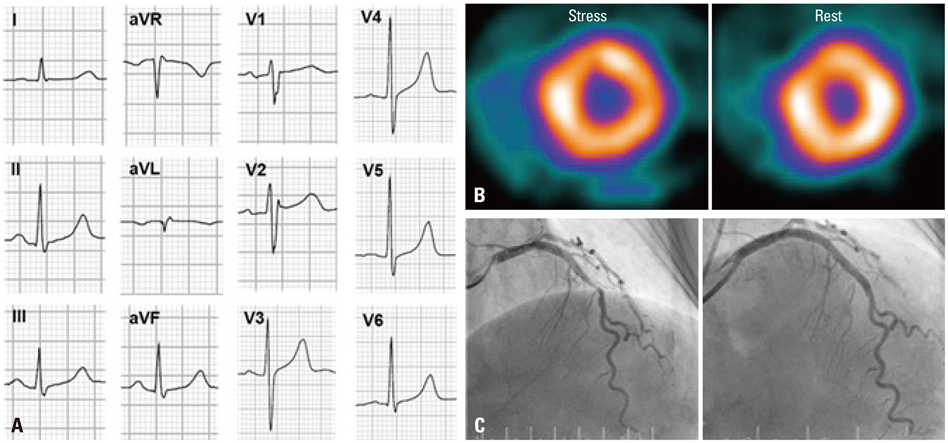
Of 570 consecutive CAD patients, patients with and without ER were assigned to ER group (n=139) and no ER group (n=431), respectively. Myocardial scar was evaluated using cardiac single-photon emission computed tomography.
RESULTS
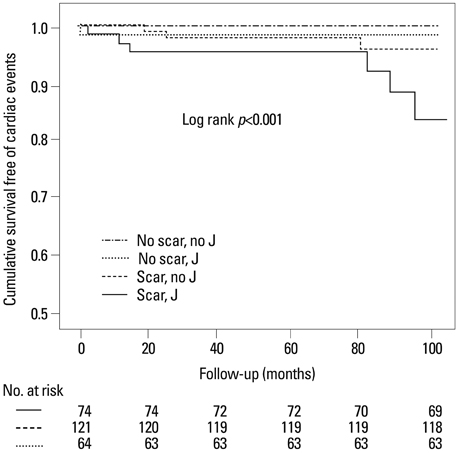
ER group had previous history of myocardial infarction (33% vs. 15%, p<0.001) and lower left ventricular ejection fraction (57+/-13% vs. 62+/-13%, p<0.001) more frequently than no-ER group. While 74 (53%) patients in ER group had myocardial scar, only 121 (28%) patients had in no-ER group (p<0.001). During follow up, 9 (7%) and 4 (0.9%) patients had cardiac events in ER and no-ER group, respectively (p=0.001). All patients with cardiac events had ER in inferior leads and horizontal/descending ST-segment. Patients with both ER in inferior leads and horizontal/descending ST variant and scar had an increased adjusted hazard ratio of cardiac events (hazard ratio 16.0; 95% confidence interval: 4.1 to 55.8; p<0.001).
CONCLUSION
ER in inferior leads with a horizontal/descending ST variant was associated with increased risk of cardiac events. These findings suggest that ER in patients with CAD may be related to myocardial scar rather than pure ion channel problem.
MeSH Terms
Figure
Reference
-
1. Goldman MJ. RS-T segment elevation in mid- and left precordial leads as a normal variant. Am Heart J. 1953; 46:817–820.
Article2. Klatsky AL, Oehm R, Cooper RA, Udaltsova N, Armstrong MA. The early repolarization normal variant electrocardiogram: correlates and consequences. Am J Med. 2003; 115:171–177.
Article3. Haïssaguerre M, Chatel S, Sacher F, Weerasooriya R, Probst V, Loussouarn G, et al. Ventricular fibrillation with prominent early repolarization associated with a rare variant of KCNJ8/KATP channel. J Cardiovasc Electrophysiol. 2009; 20:93–98.4. Nam GB, Kim YH, Antzelevitch C. Augmentation of J waves and electrical storms in patients with early repolarization. N Engl J Med. 2008; 358:2078–2079.
Article5. Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D, et al. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects: incidence and clinical significance. J Am Coll Cardiol. 2008; 52:1231–1238.
Article6. Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen HA, et al. Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med. 2009; 361:2529–2537.
Article7. Tikkanen JT, Junttila MJ, Anttonen O, Aro AL, Luttinen S, Kerola T, et al. Early repolarization: electrocardiographic phenotypes associated with favorable long-term outcome. Circulation. 2011; 123:2666–2673.8. Kataoka H. Electrocardiographic patterns of the Brugada syndrome in right ventricular infarction/ischemia. Am J Cardiol. 2000; 86:1056.
Article9. Indik JH, Ott P, Butman SM. Syncope with ST-segment abnormalities resembling Brugada syndrome due to reversible myocardial ischemia. Pacing Clin Electrophysiol. 2002; 25:1270–1273.
Article10. Jastrzebski M, Kukla P. Ischemic J wave: novel risk marker for ventricular fibrillation? Heart Rhythm. 2009; 6:829–835.
Article11. Yan GX, Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation. 1996; 93:372–379.
Article12. Hlaing T, DiMino T, Kowey PR, Yan GX. ECG repolarization waves: their genesis and clinical implications. Ann Noninvasive Electrocardiol. 2005; 10:211–223.
Article13. Patel RB, Ng J, Reddy V, Chokshi M, Parikh K, Subacius H, et al. Early repolarization associated with ventricular arrhythmias in patients with chronic coronary artery disease. Circ Arrhythm Electrophysiol. 2010; 3:489–495.
Article14. Oh CM, Oh J, Shin DH, Hwang HJ, Kim BK, Pak HN, et al. Early repolarization pattern predicts cardiac death and fatal arrhythmia in patients with vasospastic angina. Int J Cardiol. 2013; 167:1181–1187.
Article15. Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005; 111:659–670.
Article16. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992; 20:1391–1396.
Article17. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
Article18. Haïssaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008; 358:2016–2023.
Article19. Gussak I, Antzelevitch C. Early repolarization syndrome: clinical characteristics and possible cellular and ionic mechanisms. J Electrocardiol. 2000; 33:299–309.
Article20. Myerburg RJ, Kessler KM, Mallon SM, Cox MM, deMarchena E, Interian A Jr, et al. Life-threatening ventricular arrhythmias in patients with silent myocardial ischemia due to coronary-artery spasm. N Engl J Med. 1992; 326:1451–1455.
Article21. Amsterdam EA. Relation of silent myocardial ischemia to ventricular arrhythmias and sudden death. Am J Cardiol. 1988; 62:24I–27I.
Article22. Castle CH, Keane WM. Electrocardiographic "peri-infarction block". A clinical and pathologic correlation. Circulation. 1965; 31:403–408.23. Scherlag BJ, Gunn CG, Berbari EJ, Lazzara R. Peri-infarction block (1950)-late potentials (1980): their relationship, significance and diagnostic implications. Am J Cardiol. 1985; 55:839–841.
Article24. Furukawa Y, Yamada T, Morita T, Iwasaki Y, Kawasaki M, Kikuchi A, et al. Early repolarization pattern associated with sudden cardiac death: long-term follow-up in patients with chronic heart failure. J Cardiovasc Electrophysiol. 2013; 24:632–639.
Article25. Litovsky SH, Antzelevitch C. Transient outward current prominent in canine ventricular epicardium but not endocardium. Circ Res. 1988; 62:116–126.
Article26. Kim BK, Yoon JH, Shin DH, Kim JS, Ko YG, Choi D, et al. Prospective and systematic analysis of unexpected requests for non-cardiac surgery or other invasive procedures during the first year after drug-eluting stent implantation. Yonsei Med J. 2014; 55:345–352.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute myocardial infarction in young patient probably due to Kawasaki disease
- Diagnosis of Coronary Artery Disease Using Myocardial Perfusion SPECT
- The Right Gastroepiploic Artery Graft for Coronary Artery Bypass Grafting: A 30-Year Experience
- Role of Pressure Wire in Coronary Artery Disease
- Myocardial SPECT