Experience of Advance Directives in a Hospice Center
- Affiliations
-
- 1Department of Medical Oncology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea. miongsok@catholic.ac.kr
- 2Hospice Center, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- KMID: 2129644
- DOI: http://doi.org/10.3346/jkms.2015.30.2.151
Abstract
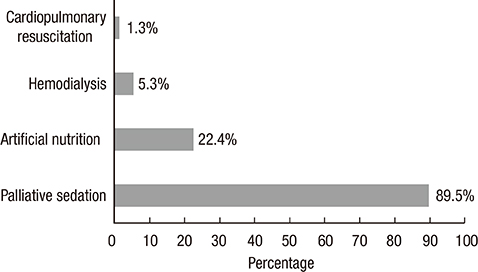
- To protect patient autonomy when confronting death, the importance of advance directives (ADs) has recently became an issue and gradually accepted in Korea. However, in real practice, ADs were not completed by patients but their families in most cases. To analyze the current situation of performing ADs, we reviewed medical charts of 214 terminal cancer patients admitted to the hospice center from October 2012 to September 2013. Seventy-six (35.5%) patients completed ADs. All ADs were completed by patients themselves. The most common reason for not completing ADs was poor physical and/or mental condition. As a proxy, the majority of patients preferred their spouses (55.3%). Few patients wanted life sustaining treatment (1.3%), however palliative sedation was accepted in 89.5%. The median timing of ADs after admission was three (0-90) days, and duration of survival since ADs was 22 (1-340) days. In conclusion, approximately one third of terminal cancer patients completed ADs by themselves. Considering that patient's poor condition is the main reason for not completing ADs, earlier discussion regarding ADs is necessary to enhance patients' participation.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Adopting Advance Directives Reinforces Patient Participation in End-of-Life Care Discussion
Ji Hyung Hong, Jung Hye Kwon, Il Kyu Kim, Jin Hee Ko, Yi-Jin Kang, Hoon-Kyo Kim
Cancer Res Treat. 2016;48(2):753-758. doi: 10.4143/crt.2015.281.Feasibility Study of Physician Orders for Life-Sustaining Treatment for Patients with Terminal Cancer
Ho Jung An, Hyun Jeong Jeon, Sang Hoon Chun, Hyun Ae Jung, Hee Kyung Ahn, Kyung Hee Lee, Min-ho Kim, Ju Hee Kim, Jaekyung Cheon, JinShil Kim, Su-Jin Koh
Cancer Res Treat. 2019;51(4):1632-1638. doi: 10.4143/crt.2019.009.Implication of the Life-Sustaining Treatment Decisions Act on End-of-Life Care for Korean Terminal Patients
Jung Sun Kim, Shin Hye Yoo, Wonho Choi, Yejin Kim, Jinui Hong, Min Sun Kim, Hye Yoon Park, Bhumsuk Keam, Dae Seog Heo
Cancer Res Treat. 2020;52(3):917-924. doi: 10.4143/crt.2019.740.A National Study of Life-Sustaining Treatments in South Korea: What Factors Affect Decision-Making?
So-Youn Park, Bomyee Lee, Jeong Yeon Seon, In-Hwan Oh
Cancer Res Treat. 2021;53(2):593-600. doi: 10.4143/crt.2020.803.The Situation of Life-Sustaining Treatment One Year after Enforcement of the Act on Decisions on Life-Sustaining Treatment for Patients at the End-of-Life in Korea: Data of National Agency for Management of Life-Sustaining Treatment
Ha Yeon Lee, Hwa Jung Kim, Jung Hye Kwon, Sun Kyung Baek, Young-Woong Won, Yu Jung Kim, Su Jin Baik, Hyewon Ryu
Cancer Res Treat. 2021;53(4):897-907. doi: 10.4143/crt.2021.327.
Reference
-
1. Brown BA. The history of advance directives: a literature review. J Gerontol Nurs. 2003; 29:4–14.2. Heo DS. Patient autonomy and advance directives in Korea. J Korean Med Assoc. 2009; 52:865–870.3. Sun DS, Chun YJ, Lee JH, Gil SH, Shim BY, Lee OK, Jung IS, Kim HK. Recognition of advance directives by advanced cancer patients and medical doctors in hospice care ward. Korean J Hosp Palliat Care. 2009; 12:20–26.4. Kwon SH, Im SH, Cho KW, Cho E, Yoon SJ, Oh SY. Most advance directives written by patients with advanced cancer or their proxies request only minimally invasive treatments during end-of-life care. Am J Hosp Palliat Care. 2012; 29:622–626.5. Shim BY, Hong SI, Park JM, Cho HJ, Ok JS, Kim SY, Han SA, Lee OK, Kim HK. DNR (Do-Not-Resuscitate) order for terminal cancer patients at hospice ward in Korea. Korean J Hosp Palliat Care. 2004; 7:232–237.6. Oh DY, Kim JH, Kim DW, Im SA, Kim TY, Heo DS, Bang YJ, Kim NK. CPR or DNR? End-of-life decision in Korean cancer patients: a single center's experience. Support Care Cancer. 2006; 14:103–108.7. Kim DY, Lee KE, Nam EM, Lee HR, Lee KW, Kim JH, Lee JS, Lee SN. Do-not-resuscitate orders for terminal patients with cancer in teaching hospitals of Korea. J Palliat Med. 2007; 10:1153–1158.8. Yoon HM, Choi YS, Hyun JJ. Current situation on signing advance medical directives and actual life-sustaining treatment given at a university hospital. Korean J Hosp Palliat Care. 2011; 14:91–100.9. Pautex S, Notaridis G, Déramé L, Zulian GB. Preferences of elderly cancer patients in their advance directives. Crit Rev Oncol Hematol. 2010; 74:61–65.10. Kim SS, Lee WH, Cheon J, Lee JE, Yeo K, Lee J. Preferences for advance directives in Korea. Nurs Res Pract. 2012; 2012:873892.11. Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010; 362:1211–1218.12. Keam B, Yun YH, Heo DS, Park BW, Cho CH, Kim S, Lee DH, Lee SN, Lee ES, Kang JH, et al. The attitudes of Korean cancer patients, family caregivers, oncologists, and members of the general public toward advance directives. Support Care Cancer. 2013; 21:1437–1444.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationships among Perceptions of Dying Well, Attitudes toward Advance Directives, and Preferences for Advance Directives among Elderly Living Alone
- Effects of Awareness to Well-dying, Knowledge and Attitudes toward Advance-directives on Attitude toward End-of-life Care in Nursing Students
- Influence of Advance Directives' Self-efficacy of Community-dwelling Older Adults on the Completion of Advance Directives: Mediating the Effect of Intention for Advance Directives: A Cross-Sectional Study
- The Current Status of End-of-Life Care in Korea and Legislation of Well-Dying Act
- Reliability and Validity of an Instrument Assessing Advance Directives for Nurse