J Korean Ophthalmol Soc.
2015 May;56(5):664-671. 10.3341/jkos.2015.56.5.664.
Clinical Outcomes of Nd-YAG Laser Membranotomy in Retained Host Corneal Membrane after Keratoplasty
- Affiliations
-
- 1Department of Ophthalmology, The Catholic University of Korea College of Medicine, Seoul, Korea. mskim@catholic.ac.kr
- 2Department of Ophthalmology, Inje University College of Medicine, Busan, Korea.
- KMID: 2121162
- DOI: http://doi.org/10.3341/jkos.2015.56.5.664
Abstract
- PURPOSE
To evaluate the clinical efficacy and shortcomings of neodymium-doped yttrium aluminum garnet (Nd-YAG) laser membranotomy in inadvertently retained host membrane.
METHODS
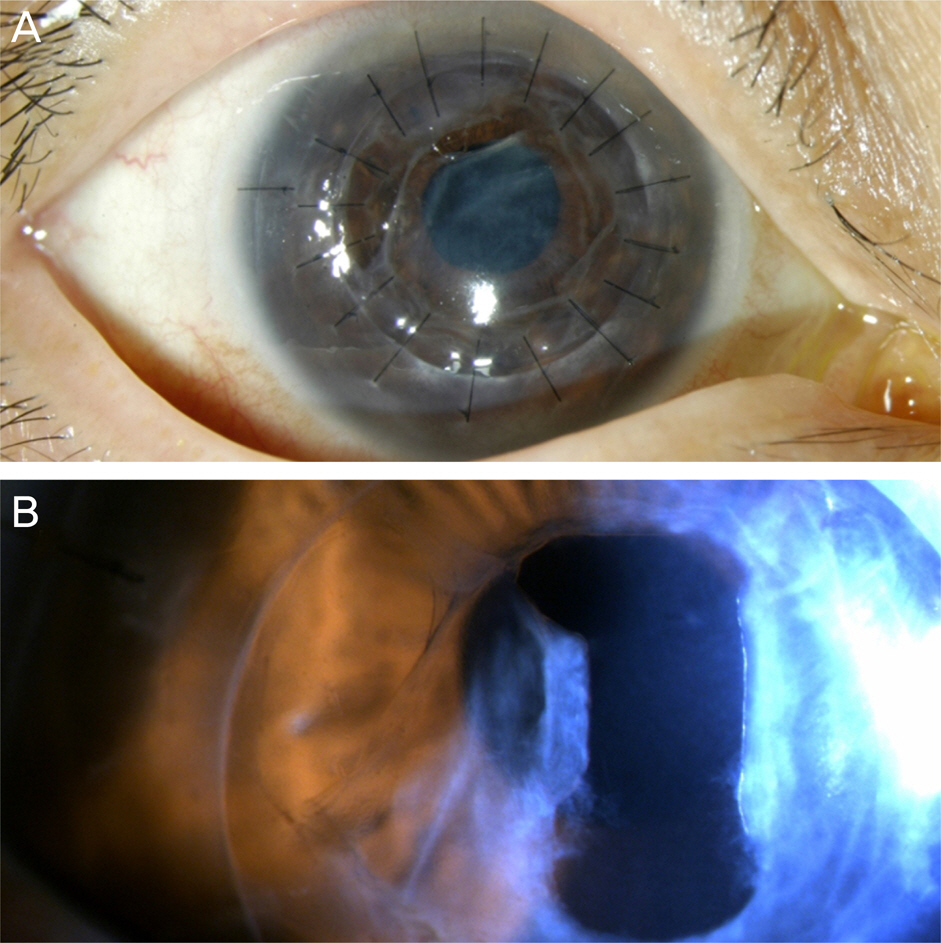
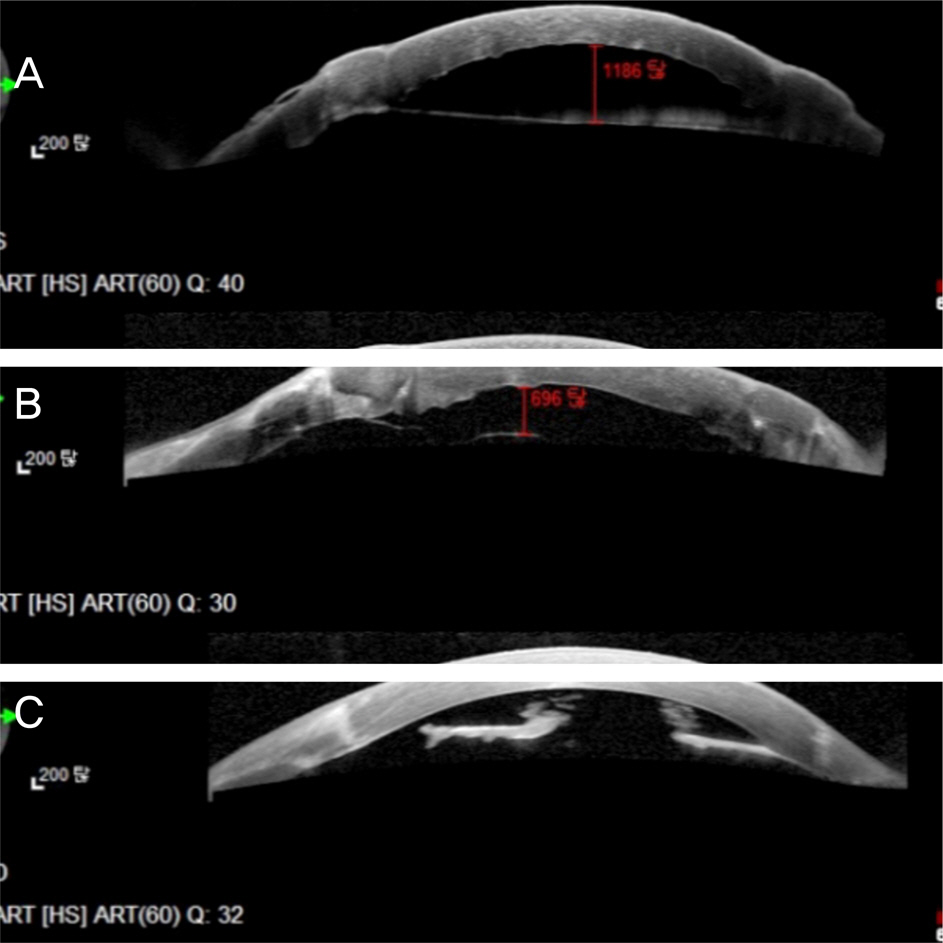
Among 742 patients who underwent penetrating keratoplasty (PKP) and deep anterior lamellar keratoplasty (DALK) surgery at Seoul St. Mary's Hospital between January 2007 and May 2013 by a single surgeon, 10 patients had a thin, opaque membrane in the anterior chamber observed under slit lamp examination and both a subjective decrease in visual acuity and decrease i best corrected visual acuity. A single surgeon performed membranotomy using the Nd-YAG laser at 4.9 months after graft surgery. In this study we compared the differences in visual acuity, endothelial cell count and correlations between distance from donor endothelium and retained host membrane and endothelial loss before and after the graft surgery.
RESULTS
Patients who had Nd-YAG laser membranotomy performed on the retained host membrane showed significant improvements in visual acuity (p = 0.039). Donor endothelial cell count was significantly reduced 1 month after Nd-YAG laser. The average distance between donor endothelium and retained host membrane was 712.0 +/- 217.5 microm. The distance and the decreased donor endothelial cell count were not statistically correlated (R2 = 0.39, p = 0.072). There were no significant complications after the laser membranotomy.
CONCLUSIONS
Inadvertently retained host membrane forms close to the donor endothelium as identified on optical coherence tomography (OCT) images. Nd-YAG laser membranotomy significantly affected clear vision but endothelial cell count loss was also observed.
MeSH Terms
Figure
Reference
-
References
1. Duke-Elder S. Text-book of Ophthalmology: Injuries. Vol. 6. London: Mosby;1954.2. Morton PL, Ormsby HL, Basu PK. Healing of endothelium and Descemet's membrane of rabbit cornea. Am J Ophthalmol. 1958; 46(1 Pt 2):62–7.
Article3. Chi HH, Teng CC, Katzin HM. Histopathology of primary endothelial-epithelial dystrophy of the cornea. Am J Ophthalmol. 1958; 45(4 Pt 1):518–35.
Article4. Stocker FW. The endothelium of the cornea and its clinical implications. Trans Am Ophthalmol Soc. 1953; 51:669–786.5. Werb A. The postgraft membrane. Int Ophthalmol Clin. 1962; 2:771–80.
Article6. Hales RH, Spencer WH. Unsuccessful penetrating keratoplasties. correlation of clinical and histologic findings. Arch Ophthalmol. 1963; 70:805–10.7. Kremer I, Dreznik A, Tessler G, Bahar I. Corneal graft failure following Nd:YAG laser membranotomy for inadvertent retained descemet's membrane after penetrating keratoplasty. Ophthalmic Surg Lasers Imaging. 2012; 43:Online. e94–8.
Article8. Brown SI, Dohlman CH, Boruchoff SA. Dislocation of descemet's membrane during keratoplasty. Am J Ophthalmol. 1965; 60:43–5.
Article9. Sinha R, Vajpayee RB, Sharma N, et al. Trypan blue assisted descemetorhexis for inadvertently retained Descemet's membranes after penetrating keratoplasty. Br J Ophthalmol. 2003; 87:654–5.
Article10. Henderson JW, Wolter JR. Separation of Descemet's membrane in keratoplasty. Am J Ophthalmol. 1968; 65:375–8.
Article11. Lazar M, Loewenstein A, Geyer O. Intentional retention of Descemet's membrane during keratoplasty. Acta Ophthalmol (Copenh). 1991; 69:111–2.
Article12. Loewenstein A, Geyer O, Lazar M. Intentional retention of Descemet's membrane in keratoplasty for the surgical treatment of bullous keratopathy. Acta Ophthalmol (Copenh). 1993; 71:280–2.
Article13. Thyagarajan S, Mearza AA, Falcon MG. Inadvertent retention of Descemet Membrane in penetrating keratoplasty. Cornea. 2006; 25:748–9.
Article14. Feng CS, Choi WS, Nam WH, Shin YJ. A case of retained descemet's membrane after penetrating keratoplasty. J Korean Ophthalmol Soc. 2013; 54:813–7.
Article15. Arenas Archila E, Ramirez Cabrera MF, Mieth Alviar A. Double Descemet's membrane in penetrating keratoplasty. Refract Corneal Surg. 1993; 9:65–6.16. Chen YP, Lai PC, Chen PY, et al. Retained Descemet's membrane after penetrating keratoplasty. J Cataract Refract Surg. 2003; 29:1842–4.
Article17. Steinemann TL, Henry K, Brown MF. Nd:YAG laser treatment of retained Descemet's membrane after penetrating keratoplasty. Ophthalmic Surg. 1995; 26:80–1.18. Patel SV, Diehl NN, Hodge DO, Bourne WM. Donor risk factors for graft failure in a 20-year study of penetrating keratoplasty. Arch Ophthalmol. 2010; 128:418–25.
Article19. Lass JH, Gal RL, Dontchev M, et al. Donor age and corneal endothelial cell loss 5 years after successful corneal transplantation. Specular microscopy ancillary study results. Ophthalmology. 2008; 115:627–32.e8.20. Waring GO 3rd, Bourne WM, Edelhauser HF, Kenyon KR. The corneal endothelium. Normal and pathologic structure and function. Ophthalmology. 1982; 89:531–90.21. Power WJ, Collum LM. Electron microscopic appearances of human corneal endothelium following Nd:YAG laser iridotomy. Ophthalmic Surg. 1992; 23:347–50.
Article22. Wu SC, Jeng S, Huang SC, Lin SM. Corneal endothelial damage after neodymium:YAG laser iridotomy. Ophthalmic Surg Lasers. 2000; 31:411–6.
Article23. Kozobolis VP, Detorakis ET, Vlachonikolis IG, Pallikaris IG. Endothelial corneal damage after neodymium:YAG laser treatment: pupillary membranectomies, iridotomies, capsulotomies. Ophthalmic Surg Lasers. 1998; 29:793–802.24. Landers J, Craig J. Decompression retinopathy and corneal oedema following Nd:YAG laser peripheral iridotomy. Clin Experiment Ophthalmol. 2006; 34:182–4.
Article25. Meyer KT, Pettit TH, Straatsma BR. Corneal endothelial damage with neodymium:YAG laser. Ophthalmology. 1984; 91:1022–8.
Article26. Vaikoussis E, Bisogiannis Z, Margaritis L. Corneal endothelial damage after Nd:YAG laser anterior capsulotomy. An experimental study on rabbits. Doc Ophthalmol. 1993; 83:279–86.27. Kerr Muir MG, Sherrard ES. Damage to the corneal endothelium during Nd/YAG photodisruption. Br J Ophthalmol. 1985; 69:77–85.
Article28. Lifshitz T, Oshry T, Rosenthal G. Retrocorneal membrane after penetrating keratoplasty. Ophthalmic Surg Lasers. 2001; 32:159–61.
Article29. Sherrard ES, Rycroft PV. Retrocorneal membranes. I. Their origin and structure. Br J Ophthalmol. 1967; 51:379–86.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Chronic Corneal Ulcer with Nd-YAG Laser
- Effects of Neodymium:YAG Laser and Tissue Plasminogen Activator on Massive Diabetic Premacular Hemorrhage
- A Case of Retained Descemet's Membrane after Penetrating Keratoplasty
- Early Result of Femtosecond Laser Assisted Descemet's Membrane Stripping Endothelial Keratoplasty
- A Case of Holmium: YAG Laser Thermal Keratoplasty to Correct Hyperopia Induced by LASIK