Tuberc Respir Dis.
2015 Jan;78(1):31-35. 10.4046/trd.2015.78.1.31.
Serious Complications after Self-expandable Metallic Stent Insertion in a Patient with Malignant Lymphoma
- Affiliations
-
- 1Department of Internal Medicine, St. Paul's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. agmante@gmail.com
- 2Department of Internal Medicine, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Internal Medicine, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea.
- KMID: 2114647
- DOI: http://doi.org/10.4046/trd.2015.78.1.31
Abstract
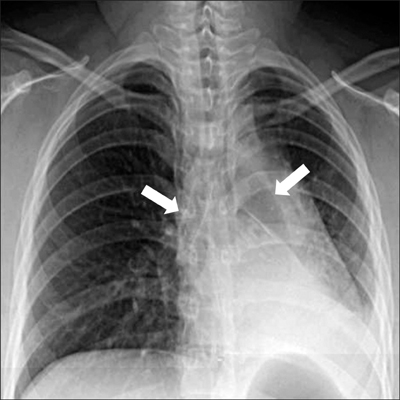
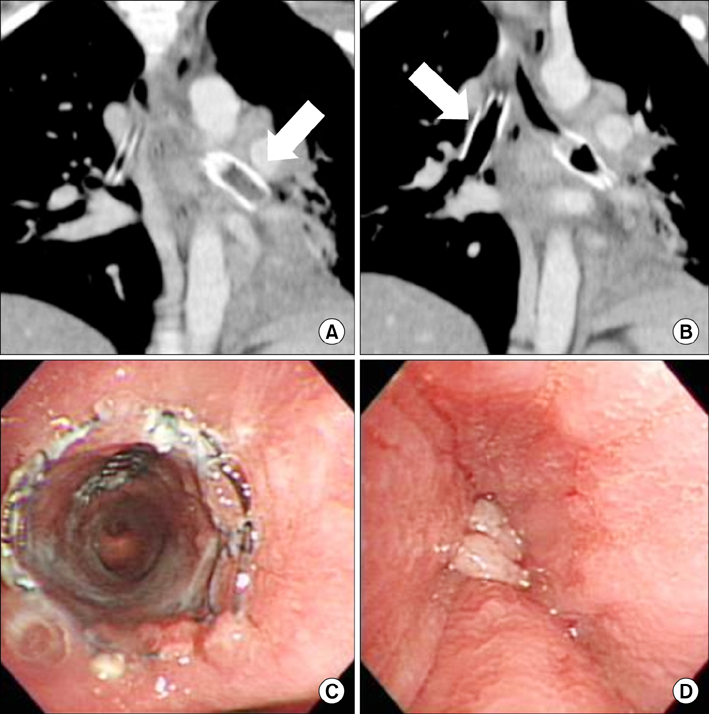
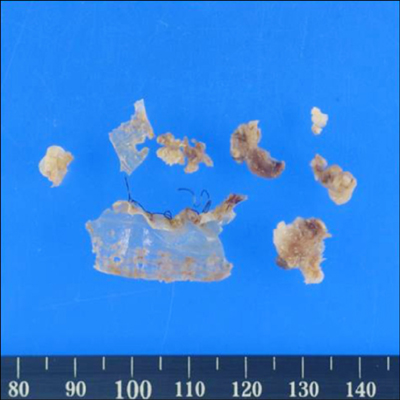
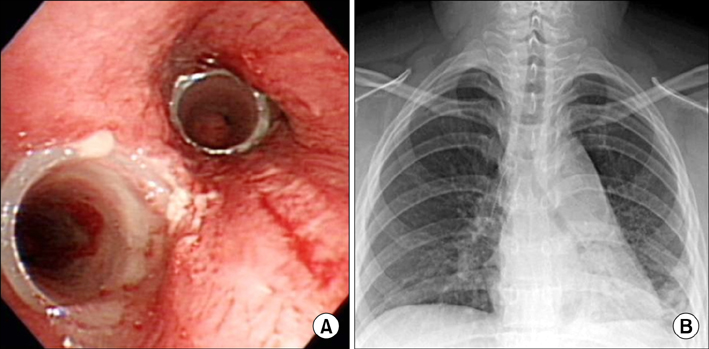
- An 18-year-old woman was evaluated for a chronic productive cough and dyspnea. She was subsequently diagnosed with mediastinal non-Hodgkin lymphoma (NHL). A covered self-expandable metallic stent (SEMS) was implanted to relieve narrowing in for both main bronchi. The NHL went into complete remission after six chemotherapy cycles, but atelectasis developed in the left lower lobe 18 months after SEMS insertion. The left main bronchus was completely occluded by granulation tissue. However, the right main bronchus and intermedius bronchus were patent. Granulation tissue was observed adjacent to the SEMS. The granulation tissue and the SEMS were excised, and a silicone stent was successfully implanted using a rigid bronchoscope. SEMS is advantageous owing to its easy implantation, but there are considerable potential complications such as severe reactive granulation, stent rupture, and ventilation failure in serious cases. Therefore, SEMS should be avoided whenever possible in patients with benign airway disease. This case highlights that SEMS implantation should be avoided even in malignant airway obstruction cases if the underlying malignancy is curable.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Case of a Temporary Endotracheal Stent for Airway Management in a Patient with Primary Thyroid Lymphoma
Young Chul Kim, Seong-Chul Yeo, Jin Pyeong Kim, Jung Je Park
Korean J Otorhinolaryngol-Head Neck Surg. 2020;63(2):85-90. doi: 10.3342/kjorl-hns.2019.00297.
Reference
-
1. Bolliger CT, Sutedja TG, Strausz J, Freitag L. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J. 2006; 27:1258–1271.2. Casal RF. Update in airway stents. Curr Opin Pulm Med. 2010; 16:321–328.3. Ernst A, Feller-Kopman D, Becker HD, Mehta AC. Central airway obstruction. Am J Respir Crit Care Med. 2004; 169:1278–1297.4. Chin CS, Litle V, Yun J, Weiser T, Swanson SJ. Airway stents. Ann Thorac Surg. 2008; 85:S792–S796.5. Ryu YJ, Kim H, Yu CM, Choi JC, Kwon YS, Kwon OJ. Use of silicone stents for the management of post-tuberculosis tracheobronchial stenosis. Eur Respir J. 2006; 28:1029–1035.6. Rafanan AL, Mehta AC. Stenting of the tracheobronchial tree. Radiol Clin North Am. 2000; 38:395–408.7. Lunn W, Feller-Kopman D, Wahidi M, Ashiku S, Thurer R, Ernst A. Endoscopic removal of metallic airway stents. Chest. 2005; 127:2106–2112.8. Noppen M, Stratakos G, D'Haese J, Meysman M, Vinken W. Removal of covered self-expandable metallic airway stents in benign disorders: indications, technique, and outcomes. Chest. 2005; 127:482–487.9. Lund ME, Force S. Airway stenting for patients with benign airway disease and the Food and Drug Administration advisory: a call for restraint. Chest. 2007; 132:1107–1108.10. Dutau H, Musani AI, Plojoux J, Laroumagne S, Astoul P. The use of self-expandable metallic stents in the airways in the adult population. Expert Rev Respir Med. 2014; 8:179–190.11. Dumon JF. A dedicated tracheobronchial stent. Chest. 1990; 97:328–332.12. Breitenbucher A, Chhajed PN, Brutsche MH, Mordasini C, Schilter D, Tamm M. Long-term follow-up and survival after Ultraflex stent insertion in the management of complex malignant airway stenoses. Respiration. 2008; 75:443–449.13. Lemaire A, Burfeind WR, Toloza E, Balderson S, Petersen RP, Harpole DH Jr, et al. Outcomes of tracheobronchial stents in patients with malignant airway disease. Ann Thorac Surg. 2005; 80:434–437.14. Chung FT, Lin SM, Chou CL, Chen HC, Liu CY, Yu CT, et al. Factors leading to obstructive granulation tissue formation after ultraflex stenting in benign tracheal narrowing. Thorac Cardiovasc Surg. 2010; 58:102–107.15. Gaissert HA, Grillo HC, Wright CD, Donahue DM, Wain JC, Mathisen DJ. Complication of benign tracheobronchial strictures by self-expanding metal stents. J Thorac Cardiovasc Surg. 2003; 126:744–747.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pyloric Obstruction Caused by Self-expandable Metallic Stent for Palliation of Malignant Dysphagia
- Usefulness of Self-expandable Metallic Stents for Malignant Colon Obstruction
- Usefulness of a Self-expandable Metallic Stent for a Malignant Colorectal Obstruction
- Self-expandable Metallic Stents for Palliative Treatment of Malignant Esophagogastric Strictures: Experiences in 103 Patients
- The use of self expandable metallic stent in the management of malignant biliary obstruction