J Korean Surg Soc.
2009 Mar;76(3):179-186. 10.4174/jkss.2009.76.3.179.
The Diagnostic Concordance of Femoral Hernia and the Factors Influencing Diagnosis
- Affiliations
-
- 1Department of Surgery, Wonkwang University School of Medicine, Iksan, Korea. docjong@wonkwang.ac.kr
- KMID: 2096541
- DOI: http://doi.org/10.4174/jkss.2009.76.3.179
Abstract
- PURPOSE
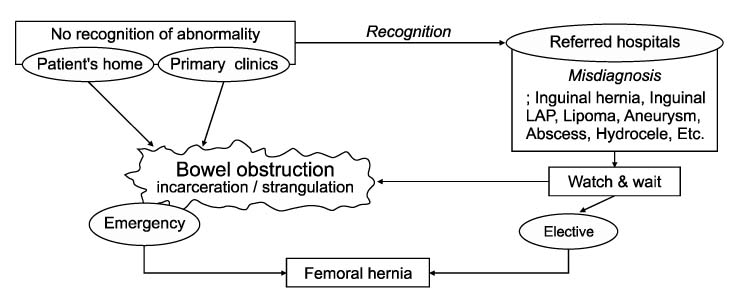
Misdiagnosis is frequent in femoral hernia as inguinal hernia. The aims of this study were to examine the diagnostic concordance and to define the factors having influence on the correct diagnosis of femoral hernia.
METHODS
Thirty-two patients who underwent femoral hernia operations were analyzed retrospectively.
RESULTS
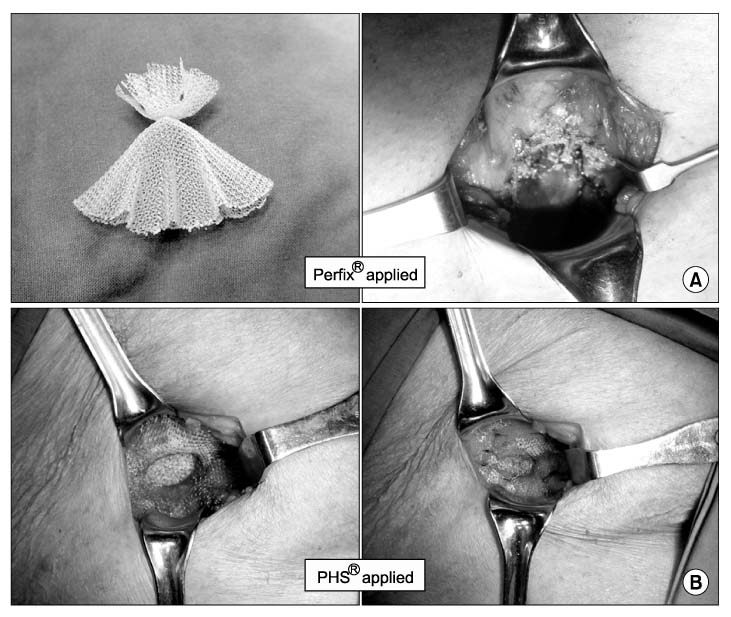
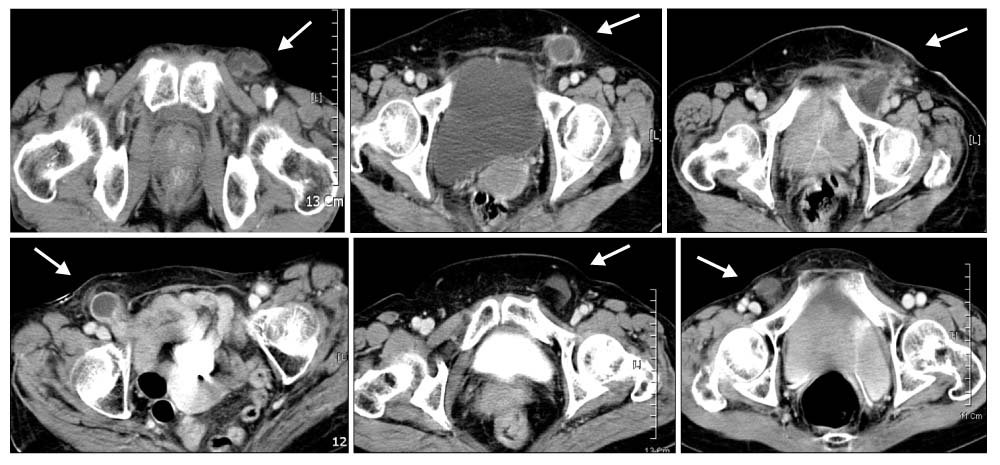
The mean age of the study subjects was 65.8+/-15.5 (36~97) and the female to male ratio was 5.4:1. The mean body mass index (BMI) was 19.8 kg/m2 (14.6~26.9 kg/m2). Twelve patients (37.5%) showed pre- and post-operative diagnostic concordance and 20 patients (62.5%) did not. Among the 20 misdiagnosed cases, 16 cases were misdiagnosed as inguinal hernia, 2 cases as lipoma, and 1 case as lymphadenopathy. The factors related to the correct diagnosis of femoral hernias were associated with groin mass (96.9%, 31/32: 23 painless and 8 painful), size fluctuation of mass (cyclic wax and wane pattern) (84.4%, 27/32), long duration of mass (over 1 month) (75.0%, 24/32), femoral venous compression CT findings (63.6%, 14/22), and positive ultrasonographic findings (42.1%, 8/19). Emergency operation was done in 12 cases (37.5%). Incarceration was found in 23 cases (71.9%) and most of the incarcerated organs were omental fat (11 cases) and small bowel (10 cases). Bowel resection was done in 4 cases and 2 patients combined inguinal hernia.
CONCLUSION
Through the careful taking of medical history and physical examination, physicians can achieve the correct diagnosis and can also decrease the frequency of emergency operations and their related complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Richards AT, Quinn TH, Fitzgibbons RJ. Greenfield LJ , editor. Abdominal wall hernias. Surgery: Scientific Principles and Practice. 2001. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;1185–1223.2. Kemler MA, Oostvogel HJ. Femoral hernia: is a conservative policy justified? Eur J Surg. 1997. 163:187–190.3. Naude GP, Ocon S, Bongard F. Femoral hernia: the dire consequences of a missed diagnosis. Am J Emerg Med. 1997. 15:680–682.4. Nilsson H, Stylianidis G, Haapamaki M, Nilsson E, Nordin P. Mortality after groin hernia surgery. Ann Surg. 2007. 245:656–660.5. Brittenden J, Heys SD, Eremin O. Femoral hernia: mortality and morbidity following elective and emergency surgery. J R Coll Surg Edinb. 1991. 36:86–88.6. Sandblom G, Haapaniemi S, Nilsson E. Femoral hernias: a register analysis of 588 repairs. Hernia. 1999. 3:131–134.7. Buchin P, Steinau G, Ophoff K, Dreuw B, Truong S, Schumpelick V. Femoral hernia in childhood: evaluation of sonography as a diagnostic aid. Hernia. 1999. 3:19–21.8. Mikkelsen T, Bay-Nielsen M, Kehlet H. Risk of femoral hernia after inguinal herniorrhaphy. Br J Surg. 2002. 89:486–488.9. Bendavid R. Femoral hernias: primary versus recurrence. Int Surg. 1989. 74:99–100.10. Rhind JR. Lateral femoral hernia. J R Coll Surg Edinb. 1971. 16:299–300.11. Ponka JL, Brush BE. Problem of femoral hernia. Arch Surg. 1971. 102:417–423.12. Quill DS, Devlin HB, Plant JA, Denham KR, McNay RA, Morris D. Surgical operation rates: a twelve year experience in Stockton on Tees. Ann R Coll Surg Engl. 1983. 65:248–253.13. Malek S, Torella F, Edwards PR. Emergency repair of groin herniae: outcome and implications for elective surgery waiting times. Int J Clin Pract. 2004. 58:207–209.14. Chen KC, Chu CC, Chou TY, Wu CJ. Ultrasonography for inguinal hernias in boys. J Pediatr Surg. 1998. 33:1784–1787.15. Chou TY, Chu CC, Diau GY, Wu CJ, Gueng MK. Inguinal hernia in children: US versus exploratory surgery and intraoperative contralateral laparoscopy. Radiology. 1996. 201:385–388.16. Zhang GQ, Sugiyama M, Hagi H, Urata T, Shimamori N, Atomi Y. Groin hernias in adults: value of color Doppler sonography in their classification. J Clin Ultrasound. 2001. 29:429–434.17. Bradley M, Morgan D, Pentlow B, Roe A. The groin hernia - an ultrasound diagnosis? Ann R Coll Surg Engl. 2003. 85:178–180.18. Delabrousse E, Denue PO, Aubry S, Sarlieve P, Mantion GA, Kastler BA. The pubic tubercle: a CT landmark in groin hernia. Abdom Imaging. 2007. 32:803–806.19. Ianora AA, Midiri M, Vinci R, Rotondo A, Angelelli G. Abdominal wall hernias: imaging with spiral CT. Eur Radiol. 2000. 10:914–919.20. Zarvan NP, Lee FT Jr, Yandow DR, Unger JS. Abdominal hernias: CT findings. AJR Am J Roentgenol. 1995. 164:1391–1395.21. Cherian PT, Parnell AP. The diagnosis and classification of inguinal and femoral hernia on multisection spiral CT. Clin Radiol. 2008. 63:184–192.22. Suzuki S, Furui S, Okinaga K, Sakamoto T, Murata J, Furukawa A, et al. Differentiation of femoral versus inguinal hernia: CT findings. AJR Am J Roentgenol. 2007. 189:W78–W83.23. Alimoglu O, Kaya B, Okan I, Dasiran F, Guzey D, Bas G, et al. Femoral hernia: a review of 83 cases. Hernia. 2006. 10:70–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Importance of Femoral Hernia in Children
- Clinical Analysis of Femoral Hernia in Adult
- Totally Extraperitoneal (TEP) Approach for Femoral Hernia
- Comparison of Inguinal Hernia in both Sexes and Laparoscopic Surgery for Female Patients
- The Clinical Characteristics and Recent Methods of Treatment in Femoral Hernia