Korean J Obstet Gynecol.
2012 Feb;55(2):76-82. 10.5468/KJOG.2012.55.2.76.
The prognostic significance of lymphovascular space involvement in patients with uterine-confined endometrioid endometrial cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Gachon University Gil Hospital, Gachon University of Medicine and Science, Incheon, Korea. pcy0523@unitel.co.kr
- KMID: 2078118
- DOI: http://doi.org/10.5468/KJOG.2012.55.2.76
Abstract
OBJECTIVE
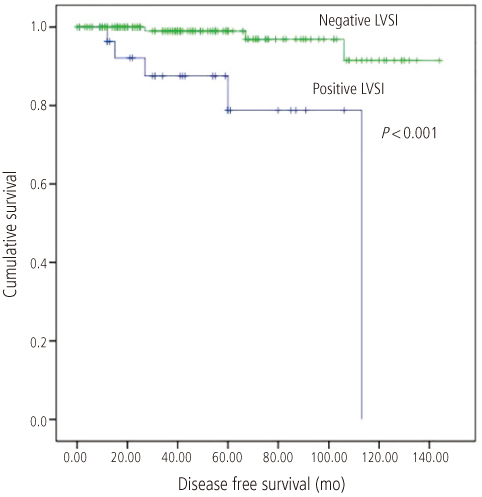
We evaluated whether or not lymphovascular space involvement (LVSI) is a risk factor for the relapse of disease in patients with uterine-confined endometrioid endometrial cancer.
METHODS
A retrospective chart review was carried out of 165 patients with uterine confined endoemtrioid-type endometrial cancer after initial treatments including total abdominal or laparoscopic hysterectomy, and bilateral salpingo-oophorectomy, with or without lymphadenectomy, peritoneal washing between 1998 and 2010. The patients with positive peritoneal cytology were not excluded.
RESULTS
The median age was 52 years (range, 26 to 81 years) with a median follow-up of 46 months (range, 1 to 144 months). One hundred twenty-four patients (75.2%) received no adjuvant treatment, 41 patients (24.8%) received adjuvant treatment including platinum-based chemotherapy, radiation therapy, and chemoradiation. LVSI was present in 29 patients (17.6%). Eight patients (4.8%) developed recurrences. Using univariate analysis, age>50 years, the tumor grade, and LVSI were found to relate to recurrence-free survival (P < 0.05). LVSI was associated with other prognostic factors such as old age, a higher tumor grade, and deeper myometrial invasion. But multivariate analysis showed no significance. LVSI was not an independent factor to predict recurrence (P = 0.093).
CONCLUSION
LVSI was associated with an increased likelihood of recurrence via univariate analysis in patients with uterine-confined endometrioid endometrial cancer. Multivariate analysis showed no statistical significance. The presence of LVSI seems to have no effect, in and of itself, to alter the treatment plan or to predict the prognosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Morrow CP, Bundy BN, Kurman RJ, Creasman WT, Heller P, Homesley HD, et al. Relationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: a Gynecologic Oncology Group study. Gynecol Oncol. 1991. 40:55–65.2. Mariani A, Webb MJ, Keeney GL, Lesnick TG, Podratz KC. Surgical stage I endometrial cancer: predictors of distant failure and death. Gynecol Oncol. 2002. 87:274–280.3. Zaino RJ, Kurman RJ, Diana KL, Morrow CP. Pathologic models to predict outcome for women with endometrial adenocarcinoma: the importance of the distinction between surgical stage and clinical stage: a Gynecologic Oncology Group study. Cancer. 1996. 77:1115–1121.4. Roman LD, Felix JC, Muderspach LI, Varkey T, Burnett AF, Qian D, et al. Influence of quantity of lymph-vascular space invasion on the risk of nodal metastases in women with early-stage squamous cancer of the cervix. Gynecol Oncol. 1998. 68:220–225.5. O'Hanlan KA, Kargas S, Schreiber M, Burrs D, Mallipeddi P, Longacre T, et al. Ovarian carcinoma metastases to gastrointestinal tract appear to spread like colon carcinoma: implications for surgical resection. Gynecol Oncol. 1995. 59:200–206.6. Paladini D, Cross P, Lopes A, Monaghan JM. Prognostic significance of lymph node variables in squamous cell carcinoma of the vulva. Cancer. 1994. 74:2491–2496.7. Katz A, Strom EA, Buchholz TA, Theriault R, Singletary SE, McNeese MD. The influence of pathologic tumor characteristics on locoregional recurrence rates following mastectomy. Int J Radiat Oncol Biol Phys. 2001. 50:735–742.8. Hanson MB, van Nagell JR Jr, Powell DE, Donaldson ES, Gallion H, Merhige M, et al. The prognostic significance of lymph-vascular space invasion in stage I endometrial cancer. Cancer. 1985. 55:1753–1757.9. Creasman WT, Morrow CP, Bundy BN, Homesley HD, Graham JE, Heller PB. Surgical pathologic spread patterns of endometrial cancer. A Gynecologic Oncology Group Study. Cancer. 1987. 60:2035–2041.10. Boronow RC, Morrow CP, Creasman WT, Disaia PJ, Silverberg SG, Miller A, et al. Surgical staging in endometrial cancer: clinical-pathologic findings of a prospective study. Obstet Gynecol. 1984. 63:825–832.11. Cohn DE, Horowitz NS, Mutch DG, Kim SM, Manolitsas T, Fowler JM. Should the presence of lymphvascular space involvement be used to assign patients to adjuvant therapy following hysterectomy for unstaged endometrial cancer? Gynecol Oncol. 2002. 87:243–246.12. Mariani A, Dowdy SC, Keeney GL, Haddock MG, Lesnick TG, Podratz KC. Predictors of vaginal relapse in stage I endometrial cancer. Gynecol Oncol. 2005. 97:820–827.13. Mariani A, Webb MJ, Keeney GL, Aletti G, Podratz KC. Predictors of lymphatic failure in endometrial cancer. Gynecol Oncol. 2002. 84:437–442.14. Briet JM, Hollema H, Reesink N, Aalders JG, Mourits MJ, ten Hoor KA, et al. Lymphvascular space involvement: an independent prognostic factor in endometrial cancer. Gynecol Oncol. 2005. 96:799–804.15. Ambros RA, Kurman RJ. Combined assessment of vascular and myometrial invasion as a model to predict prognosis in stage I endometrioid adenocarcinoma of the uterine corpus. Cancer. 1992. 69:1424–1431.16. Tsuruchi N, Kaku T, Kamura T, Tsukamoto N, Tsuneyoshi M, Akazawa K, et al. The prognostic significance of lymphovascular space invasion in endometrial cancer when conventional hemotoxylin and eosin staining is compared to immunohistochemical staining. Gynecol Oncol. 1995. 57:307–312.17. Kadar N, Malfetano JH, Homesley HD. Determinants of survival of surgically staged patients with endometrial carcinoma histologically confined to the uterus: implications for therapy. Obstet Gynecol. 1992. 80:655–659.18. Inoue Y, Obata K, Abe K, Ohmura G, Doh K, Yoshioka T, et al. The prognostic significance of vascular invasion by endometrial carcinoma. Cancer. 1996. 78:1447–1451.19. Nishiya M, Sakuragi N, Hareyama H, Ebina Y, Furuya M, Oikawa M, et al. Cox multivariate regression models for estimating prognosis of patients with endometrioid adenocarcinoma of the uterine corpus who underwent thorough surgical staging. Int J Cancer. 1998. 79:521–525.20. Mariani A, Webb MJ, Keeney GL, Aletti G, Podratz KC. Assessment of prognostic factors in stage IIIA endometrial cancer. Gynecol Oncol. 2002. 86:38–44.21. Desrosiers L, Fadare O, Xiao ZF, Dresser K, Wang SA. Lymphovascular space invasion does not predict vaginal relapses in stage I endometrioid adenocarcinoma of the endometrium. Ann Diagn Pathol. 2008. 12:112–117.22. Croog VJ, Abu-Rustum NR, Barakat RR, Alektiar KM. Adjuvant radiation for early stage endometrial cancer with lymphovascular invasion. Gynecol Oncol. 2008. 111:49–54.23. Johnson N, Cornes P. Survival and recurrent disease after postoperative radiotherapy for early endometrial cancer: systematic review and meta-analysis. BJOG. 2007. 114:1313–1320.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic significance of lymphovascular space invasion in patients with endometrioid endometrial cancer: a retrospective study from a single center
- An Analysis of Clinicopathologic Prognostic Factors Affecting Survival in Patients with Uterine Endometrial Cancer
- Comparison of three different risk-stratification models for predicting lymph node involvement in endometrioid endometrial cancer clinically confined to the uterus
- A Case of Papillary Serous Carcinoma of Endometrium
- Impact of adjuvant treatment on survival in patients with 2023 FIGO stage IIC endometrial cancer: a retrospective analysis from two tertiary centers in Korea and Taiwan