Korean J Pain.
2013 Oct;26(4):374-378. 10.3344/kjp.2013.26.4.374.
The Effect of Ultrasound-guided TAPB on Pain Management after Total Abdominal Hysterectomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Amiralmomenin Hospital, Tehran, Islamic Republic of Iran. helengharaee@yahoo.com
- 2Anesthesiology and Pain Department, Rasoul-Akram Hospital, Tehran, Islamic Republic of Iran.
- 3Genycology Department, Rasoul-Akram Hospital, Tehran, Islamic Republic of Iran.
- 4Minimally Invasive Surgery Research Centre, Tehran University of Medical Sciences, Tehran, Islamic Republic of Iran.
- KMID: 2074046
- DOI: http://doi.org/10.3344/kjp.2013.26.4.374
Abstract
- BACKGROUND
Incisional pain is particularly troublesome after hysterectomy. A method called transversus abdominis plane block (TAPB) has shown promise in managing postoperative pain. In this study, we evaluated the analgesic efficacy of ultrasound-guided TAPB after hysterectomy at different time points and at each time point separately for 48 hours.
METHODS
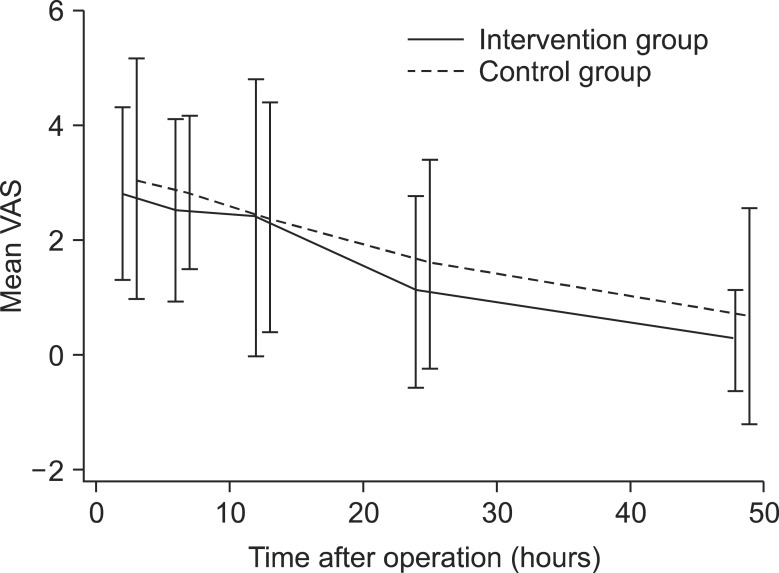
Forty-two patients (ASA I, II) who were electively chosen to undergo total abdominal hysterectomy were divided into 2 groups, control (group C) and intervention (group I). Twenty-one patients underwent TAPB (group I) and 21 patients received only the standard treatment with a fentanyl pump (group C). Both groups received standard general anesthesia. For patients in group I, following the surgery and before emergence from anesthesia, 0.5 mg/kg of ropivacaine 0.2% (about 20 cc) was injected bilaterally between the internal oblique and transverse abdominis muscles using sonography. Pain scores using the Visual Analogue Scale (VAS) and drug consumption were measured at 2, 6, 12, 24, and 48 hours after TAPB.
RESULTS
There were no significant differences in demographics between the two groups. VAS scores appeared to be lower in group I, although there was no interaction with time when we compared mean VAS measurements at different time points between group I and group C (P > 0.05). The amount of fentanyl flow was consistently higher in group C, but when we compared the two groups at each time point separately, the observed difference was not statistically significant (P < 0.053). The incidence of vomiting was 10% in group I and 28% in group C. There were no complaints of itching, and sedation score was 0 to 3. There were no complications.
CONCLUSIONS
This study showed that TAPB did not result in a statistically significant decrease in VAS scores at different time points. TAPB did lead to decreased fentanyl flow, but when we compared the two groups at each time point separately, the observed difference was not statistically significant.
MeSH Terms
Figure
Cited by 1 articles
-
Serratus Anterior Plane (SAP) Block Used for Thoracotomy Analgesia: A Case Report
Korgün Okmen, Burcu Metin Okmen, Serkan Uysal
Korean J Pain. 2016;29(3):189-192. doi: 10.3344/kjp.2016.29.3.189.
Reference
-
1. Stanley G, Appadu B, Mead M, Rowbotham DJ. Dose requirements, efficacy and side effects of morphine and pethidine delivered by patient-controlled analgesia after gynaecological surgery. Br J Anaesth. 1996; 76:484–486. PMID: 8652316.
Article2. Woodhouse A, Mather LE. The effect of duration of dose delivery with patient-controlled analgesia on the incidence of nausea and vomiting after hysterectomy. Br J Clin Pharmacol. 1998; 45:57–62. PMID: 9489595.
Article3. Ng A, Swami A, Smith G, Davidson AC, Emembolu J. The analgesic effects of intraperitoneal and incisional bupivacaine with epinephrine after total abdominal hysterectomy. Anesth Analg. 2002; 95:158–162. PMID: 12088961.
Article4. Netter FH. Back and spinal cord. In : Netter FH, editor. Atlas of human anatomy. (NJ): Ciba-Geigy Corporation;1989. p. 145–155.5. McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007; 104:193–197. PMID: 17179269.
Article6. McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008; 106:186–191. PMID: 18165577.
Article7. O'Donnell BD, McDonnell JG, McShane AJ. The transversus abdominis plane (TAP) block in open retropubic prostatectomy. Reg Anesth Pain Med. 2006; 31:91. PMID: 16418039.8. Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008; 107:2056–2060. PMID: 19020158.
Article9. Shibata Y, Sato Y, Fujiwara Y, Komatsu T. Transversus abdominis plane block. Anesth Analg. 2007; 105:883. PMID: 17717265.
Article10. McDonnell JG, O'Donnell BD, Farrell T, Gough N, Tuite D, Power C, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007; 32:399–404. PMID: 17961838.
Article11. Russon K, Blanco R. Ultrasound-guided transversus abdominal plane block. In : Bigeleisen PE, editor. Ultrasound guided regional anesthesia and pain medicine. Philadelphia (PA): Lippincott Williams & Wilkins Health;2010. p. 93–96.12. Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001; 56:1024–1026. PMID: 11576144.
Article13. Hebbard P. Subcostal transversus abdominis plane block under ultrasound guidance. Anesth Analg. 2008; 106:674–675. PMID: 18227342.
Article14. Niraj G, Kelkar A, Jeyapalan I, Graff-Baker P, Williams O, Darbar A, et al. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011; 66:465–471. PMID: 21457153.
Article15. Mokini Z. Transverse abdominal plexus block. In : Mokini Z, Vitale G, Costantini A, Fumagalli R, editors. The flying publisher guide to ultrasound blocks for the anterior abdominal wall: principles and implementation for adult and pediatric surgery. Wuppertal: Flying Publisher;2011. p. 35.16. Kanazi GE, Aouad MT, Abdallah FW, Khatib MI, Adham AM, Harfoush DW, et al. The analgesic efficacy of subarachnoid morphine in comparison with ultrasound-guided transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2010; 111:475–481. PMID: 20488929.
Article17. Belavy D, Cowlishaw PJ, Howes M, Phillips F. Ultrasound-guided transversus abdominis plane block for analgesia after caesarean delivery. Br J Anaesth. 2009; 103:726–730. PMID: 19700776.
Article18. El Bayoumy R, Khan O, King E, Wainwright D, Sadek S. Trans-abdominal plane (TAP) block analgesia in day case laparoscopic cholecystectomy - a prospective study: 14AP12-6. Eur J Anaesth. 2010; 27:222.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The analgesic effect of ultrasound-guided transverse abdominis plane block after laparoscopic totally extraperitoneal hernia repair
- Ultrasound-guided interventions for spinal pain
- Endoscopic ultrasound-guided celiac plexus neurolysis for managing abdominal pain related with advanced cancer
- Ultrasound Guided Transversus Abdominis Plane Block for Anterior Cutaneous Nerve Entrapment Syndrome
- Real-time ultrasound guided thoracic epidural catheterization: a technical review