The Analgesic Effect of Nefopam with Fentanyl at the End of Laparoscopic Cholecystectomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, Wonkwang University, Iksan, Korea. ykfolder@wku.ac.kr
- KMID: 2074044
- DOI: http://doi.org/10.3344/kjp.2013.26.4.361
Abstract
- BACKGROUND
Nefopam is a centrally acting analgesic that is used to control pain. The aim of this study was to find an appropriate dose of nefopam that demonstrates an analgesic effect when administered in continuous infusion with fentanyl at the end of laparoscopic cholecystectomy.
METHODS
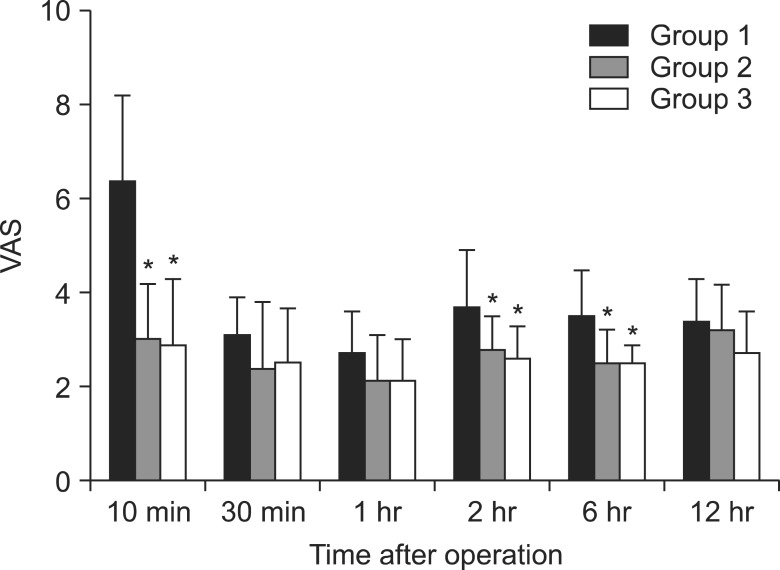
Ninety patients scheduled for laparoscopic cholecystectomy were randomly assigned to receive analgesia with fentanyl alone (50 microg, Group 1, n = 30), or with fentanyl in combination with nefopam 20 mg (Group 2, n = 30) or in combination with nefopam 40 mg (Group 3, n = 30) at the end of surgery. Pain and side effects were evaluated at 10 minutes, 30 minutes, 1 hour, 2 hours, 6 hours, and 12 hours after arrival in the post-anesthesia care unit (PACU).
RESULTS
Pain was statistically significantly lower in Groups 2 and 3 than in Group 1 at 10 minutes, 2 hours, and 6 hours after arrival in the PACU. Nausea was statistically significantly lower in Group 2 than in Groups 1 and 3 at 10 minutes after arrival in the PACU. Shivering was statistically significantly lower in Groups 2 and 3 than in Group 1 at 10 minutes after arrival in the PACU.
CONCLUSIONS
Nefopam is a drug that can be safely used as an analgesic after surgery, and its side effects can be reduced when fentanyl 50 microg is injected with nefopam 20 mg.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Effects on postoperative nausea and vomiting of nefopam versus fentanyl following bimaxillary orthognathic surgery: a prospective double-blind randomized controlled trial
Eunhye Choi, Myong-Hwan Karm, Eunsun So, Yoon Ji Choi, Sookyung Park, Yul Oh, Hye Joo Yun, Hyun Jeong Kim, Kwang-Suk Seo
J Dent Anesth Pain Med. 2019;19(1):55-66. doi: 10.17245/jdapm.2019.19.1.55.Medications in Treatment of Postherpetic Neuralgia
Sang Wook Shin
Korean J Pain. 2014;27(1):1-2. doi: 10.3344/kjp.2014.27.1.1.The Effect of Nefopam on Postoperative Fentanyl Consumption: A Randomized, Double-blind Study
Jee Youn Moon, Sang Sik Choi, Shin Young Lee, Mi Kyung Lee, Jung Eun Kim, Ji Eun Lee, So Hyun Lee
Korean J Pain. 2016;29(2):110-118. doi: 10.3344/kjp.2016.29.2.110.Use of Nefopam in Perioperative Pain Management; Keeping Nefopam in between
Jeong Il Choi
Korean J Pain. 2016;29(2):71-72. doi: 10.3344/kjp.2016.29.2.71.
Reference
-
1. Klohs MW, Draper MD, Petracek FJ, Ginzel KH, Ré ON. Benzoxazocines: a new chemical class of centrally acting skeletal muscle relaxants. Arzneimittelforschung. 1972; 22:132–133. PMID: 5066986.2. Gassel MM, Diamantopoulos E, Petropoulos V, Hughes AC, Ballesteros ML, Ré ON. Controlled clinical trial of oral and parenteral nefopam hydrochloride. A novel and potent analgesic drug. J Clin Pharmacol. 1976; 16:34–41. PMID: 1107359.
Article3. Piercey MF, Schroeder LA. Spinal and supraspinal sites for morphine and nefopam analgesia in the mouse. Eur J Pharmacol. 1981; 74:135–140. PMID: 6276187.
Article4. Kehlet H, Dahl JB. The value of "multimodal" or "balanced analgesia" in postoperative pain treatment. Anesth Analg. 1993; 77:1048–1056. PMID: 8105724.
Article5. Kim SH, Kim SI, Ok SY, Park SY, Kim MG, Lee SJ, et al. Opioid sparing effect of low dose ketamine in patients with intravenous patient-controlled analgesia using fentanyl after lumbar spinal fusion surgery. Korean J Anesthesiol. 2013; 64:524–528. PMID: 23814653.
Article6. Cheong YK, Son Y, Song YK, Kim TY. The analgesic effect of continuous intraarticular infusion of ropivacaine and fentanyl after arthroscopic shoulder surgery. Korean J Anesthesiol. 2006; 50:449–453.
Article7. Moffat AC, Kenny GN, Prentice JW. Postoperative nefopam and diclofenac. Evaluation of their morphine-sparing effect after upper abdominal surgery. Anaesthesia. 1990; 45:302–305. PMID: 2337215.
Article8. Parker RK, Holtmann B, Smith I, White PF. Use of ketorolac after lower abdominal surgery. Effect on analgesic requirement and surgical outcome. Anesthesiology. 1994; 80:6–12. PMID: 8291731.
Article9. Dordoni PL, Della Ventura M, Stefanelli A, Iannace E, Paparella P, Rocca B, et al. Effect of ketorolac, ketoprofen and nefopam on platelet function. Anaesthesia. 1994; 49:1046–1049. PMID: 7864317.
Article10. Heel RC, Brogden RN, Pakes GE, Speight TM, Avery GS. Nefopam: a review of its pharmacological properties and therapeutic efficacy. Drugs. 1980; 19:249–267. PMID: 6991238.11. Sunshine A, Laska E. Nefopam and morphine in man. Clin Pharmacol Ther. 1975; 18:530–534. PMID: 1102231.
Article12. Tigerstedt I, Sipponen J, Tammisto T, Turunen M. Comparison of nefopam and pethidine in postoperative pain. Br J Anaesth. 1977; 49:1133–1138. PMID: 337983.
Article13. McLintock TT, Kenny GN, Howie JC, McArdle CS, Lawrie S, Aitken H. Assessment of the analgesic efficacy of nefopam hydrochloride after upper abdominal surgery: a study using patient controlled analgesia. Br J Surg. 1988; 75:779–781. PMID: 3167526.
Article14. Mimoz O, Incagnoli P, Josse C, Gillon MC, Kuhlman L, Mirand A, et al. Analgesic efficacy and safety of nefopam vs. propacetamol following hepatic resection. Anaesthesia. 2001; 56:520–525. PMID: 11412156.
Article15. Beloeil H, Delage N, Nègre I, Mazoit JX, Benhamou D. The median effective dose of nefopam and morphine administered intravenously for postoperative pain after minor surgery: a prospective randomized double-blinded isobolographic study of their analgesic action. Anesth Analg. 2004; 98:395–400. PMID: 14742377.
Article16. Van Elstraete AC, Sitbon P. Median effective dose (ED50) of paracetamol and nefopam for postoperative pain: isobolographic analysis of their antinociceptive interaction. Minerva Anestesiol. 2013; 79:232–239. PMID: 23241734.17. Tramoni G, Viale JP, Cazals C, Bhageerutty K. Morphine-sparing effect of nefopam by continuous intravenous injection after abdominal surgery by laparotomy. Eur J Anaesthesiol. 2003; 20:990–992. PMID: 14690106.
Article18. Saghaei E, Moini Zanjani T, Sabetkasaei M, Naseri K. Enhancement of antinociception by co-administrations of nefopam, morphine, and nimesulide in a rat model of neuropathic pain. Korean J Pain. 2012; 25:7–15. PMID: 22259710.
Article19. Laboureyras E, Chateauraynaud J, Richebé P, Simonnet G. Long-term pain vulnerability after surgery in rats: prevention by nefopam, an analgesic with antihyperalgesic properties. Anesth Analg. 2009; 109:623–631. PMID: 19608840.
Article20. Taniguchi Y, Ali SZ, Kimberger O, Zmoos S, Lauber R, Markstaller M, et al. The effects of nefopam on the gain and maximum intensity of shivering in healthy volunteers. Anesth Analg. 2010; 111:409–414. PMID: 20529984.
Article21. Alfonsi P, Adam F, Passard A, Guignard B, Sessler DI, Chauvin M. Nefopam, a nonsedative benzoxazocine analgesic, selectively reduces the shivering threshold in unanesthetized subjects. Anesthesiology. 2004; 100:37–43. PMID: 14695722.
Article22. Girard P, Coppé MC, Verniers D, Pansart Y, Gillardin JM. Role of catecholamines and serotonin receptor subtypes in nefopam-induced antinociception. Pharmacol Res. 2006; 54:195–202. PMID: 16750379.
Article23. Fernández-Sánchez MT, Díaz-Trelles R, Groppetti A, Manfredi B, Brini AT, Biella G, et al. Nefopam, an analogue of orphenadrine, protects against both NMDA receptor-dependent and independent veratridine-induced neurotoxicity. Amino Acids. 2002; 23:31–36. PMID: 12373515.
Article24. Cheong YK, Kim TY, Lee SW. The preventive effect on postanesthetic shivering according to the dosages of ketamine. Korean J Anesthesiol. 2008; 55:277–281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparison between ketorolac and nefopam as adjuvant analgesics for postoperative patient-controlled analgesia: a randomized, double-blind, prospective study
- Effect of nefopam for patient-controlled analgesia after laparoscopic gastrectomy
- Effects of Remifentanil and Fentanyl on Postoperative Nausea and Vomiting in Laparoscopic Cholecystectomy with using Propofol
- The Effect of Nefopam on Postoperative Fentanyl Consumption: A Randomized, Double-blind Study
- Effect of perioperative infusion of lidocaine vs. dexmedetomidine on reduced consumption of postoperative analgesics after laparoscopic cholecystectomy